
Impact of acute-care pharmacy services on health system skilled nursing locations
Highlight box
Key findings
• Acute-care-based pharmacy services can reduce medication errors, reduce drug expenses, and increase clinical interventions.
What is known and what is new?
• What is known? Pharmacists are a key part of the interdisciplinary medication therapy management team and provide positive clinical and financial benefit to the skilled nursing team.
• What is new? This groundbreaking study presents a comprehensive analysis of the optimization of pharmacy services specifically tailored for skilled nursing facilities.
What is the implication, and what should change now?
• Acute-care-based skilled nursing facilities should consider transitioning from a third-party pharmacy vendor to their acute-care pharmacy team.
Introduction
Background
The outsourcing of pharmacy skilled nursing services can result in an additional financial burden on the health care system, and it introduces the potential for increased medication-related errors and delayed medication administration. The article, high-value pharmacy enterprise (HVPE) framework, describes the following recommendation, “pharmacists are accountable for all patient medication-use needs to support safe and effective drug therapy management and should thus be included as a member of the health care team in all settings” (1). The Medicare Modernization Act of 2003 acknowledges that patients of skilled nursing facility or unit (SNF/SNU) require specialized pharmacy services to meet federal and state regulations governing the provision of medications in this setting. Traditionally, an external, for-profit, third-party pharmacy contracted vendor provides pharmacy services in this setting. These services include monthly medication clinical reviews, admission medication reconciliation, psychotropic agent usage reviews, patient education, and all medication distribution activity. A meta-analysis conducted in 2019 described mixed results when evaluating the impact of pharmacists’ services on mortality, hospitalization, and readmission rates among residents (2,3). In efforts to minimize the above, the pharmacy enterprise at a multi-center community-based health system expanded the provision of pharmacy services across the organization’s three skilled nursing locations, providing care to up to 212 patients.
Optimization of finances is a strategic priority for health care systems nationwide. An article analyzing the results of the first phase of the North Carolina Polypharmacy Initiative, a drug therapy management service, found a mean reduction in monthly drug costs (USD $30.33 per resident within skilled nursing locations, P<0.001) (3). The savings associated with these services for one month alone covered the pharmacist consultation fees associated with the service. Additionally, a meta-analysis concluded pharmacy team involvement was successful in detecting and resolving medication-related problems, which resulted in both improved prescribing practice and significant cost savings (2). These results display the financial benefit of pharmacist inclusion on the SNF team.
Transitions of care can contribute to medication errors and have an impact on the clinical continuum of care. A retrospective review found that after pharmacist intervention throughout the transitions of care from acute-care to skilled nursing process, order entry delays decreased by 68% when compared to baseline data. Patients were administered high-risk medications after scheduled administration 60% of the time prior to these services (4). This number was attributed to a delay in entering orders, reviewing orders, and procuring medication upon transfer. These delays could lead to adverse outcomes and negatively affect patient care. The article HVPE framework recommends pharmacy staff coordinate transitional and post-discharge drug therapy management for patients at high risk of readmission, which includes SNF and SNU services (1).
Clinical pharmacists are integral healthcare professionals responsible for medication therapy and patient outcomes. They collaborate closely with physicians, healthcare providers, and patients to ensure that prescribed medications contribute to optimal health outcomes. Operating across various healthcare settings, clinical pharmacists leverage their extensive knowledge of medications and disease states to effectively manage medication therapy within a multidisciplinary team. They serve as a primary source of scientifically valid information on the safe, appropriate, and cost-effective use of medications.
The role of a clinical pharmacist entails making critical decisions regarding medication therapy, including development, selection, and assessment of a patient’s health issues. Collaborating with other healthcare professionals, such as physicians and nurses, clinical pharmacists assume responsibility and accountability for providing safe, effective, and timely medication therapy. With their specialized expertise in different medicines, clinical pharmacists have a profound impact on the well-being of their patients.
In healthcare teams, clinical pharmacists play a pivotal role by enhancing screenings, diagnoses, and the management of long-term conditions in patients. They conduct thorough patient interviews encompassing medical history, social and family history, allergy records, and the use of over-the-counter drugs. This comprehensive approach ensures that medication therapy is appropriate and tailored to individual patients. Clinical pharmacists are also capable of expanding their roles, incorporating tasks such as therapeutic drug monitoring, and managing a patient’s pharmacotherapy, ultimately leading to significant improvements in patient care (5). Overall, multiple studies have consistently emphasized the positive impact of pharmacists as crucial members of the care team. Tong and colleagues conducted a systematic review that examined the clinical outcomes of clinical pharmacist roles in general medicine patients who were hospitalized. The review revealed that the involvement of clinical pharmacists led to a significant reduction in medication errors, improvement in medication appropriateness, and a decrease in the length of hospital stay (6). In a comprehensive systematic review conducted by Kaboli, 36 studies were analyzed to assess the impact of pharmacy participation in patient rounds and medication reconciliation efforts. The findings of the review indicated that the involvement of clinical pharmacists can effectively enhance medication safety, reduce medication errors, and improve patient outcomes (7).
Rationale and knowledge gap
There is robust evidence that pharmacy services within the skilled nursing setting positively affect both patient care and financial results. However, there is a knowledge gap and limited studies analyzing the optimization the skilled nursing pharmacy services to uncover the best method of maximizing clinical outcomes and minimizing the financial strain on the health system. The goals of transitioning pharmacy-based services from the for-profit contracted vendor to health system-based services included improved patient safety, decreased overall medication-related cost to the health system, improved clinical outcomes, and a benefit overall of expanded pharmacy presence within the SNF and SNU locations.
Objective
The objective of the quality improvement project is to determine the optimization of health system-based services in terms of financial benefit and transitions of care.
Methods
Prior to March 2020, Lee Health’s skilled nursing locations utilized a standalone electronic health record (EHR) that was not integrated with the rest of the health system. Medications were provided in blister pack form, which is a card of packaged doses of medications within a small, clear, or light-resistant, amber-colored plastic bubble. The contracted dispensing pharmacy dispensed the patients’ individualized medication regime in accordance with the administration date and time. In March 2020, Lee Health expanded the integrated EHR into the long-term care setting of the health system. Following EHR implementation in July 2020, the acute-care-based pharmacy team assumed responsibility for the provision of pharmacy services associated with the three skilled nursing locations. This resulted in the termination of the existing third-party vendor for pharmacy services. The skilled nursing facilities embedded within the health system have a unique opportunity to capitalize on existing acute-care pharmacy services. Outsourcing the services costs the health system additional fees in order to obtain the medication and receive the clinical services associated with providing care for SNF and SNU patients.
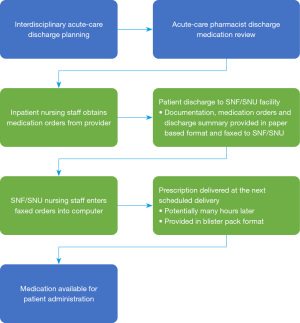
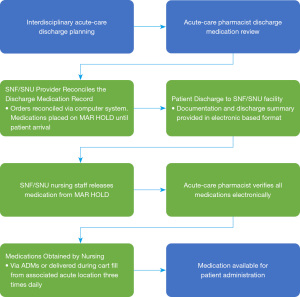
The external pharmacy-based process outlined in Figure 1 demonstrates the previous system in place for medication provision within the skilled nursing setting. In contrast, Figure 2 outlines the process following the implementation of the system-based pharmacy services. Key differences include the implementation of an integrated software system that allowed for the adoption of bar code medication administration as a patient safety tool to prevent medication errors at the point of administration, as well as the provision of pharmacy services continuous and on-site automated dispensing machines (ADMs).
In addition to the medication ADM distribution services provided internally, a full-time pharmacist was hired as a clinical specialist (1.0 full-time equivalent, or FTE) and dedicated specifically to the three skilled nursing sites. In addition, 6.0 FTEs of pharmacy technicians were added to support distribution, medication order fulfillment and restocking of ADMs. The labor costs were allocated to the respective skilled nursing locations, with dedicated technicians assigned to each campus to support and streamline workflow and medication access. Through effective budget management, a balanced approach has been maintained. It was observed that utilizing internal services, as opposed to outsourcing, resulted in improved net pharmaceutical and labor cost savings.
The dedicated clinical specialist is responsible for coordinating pharmacy services, admission reconciliation and monthly medication profile reviews. This pharmacist also works in collaboration with the onsite pharmacy support staff. This allows frequent contact with providers, nursing, administration, and patients for educational opportunities. This FTE dedicated to the SNF and SNU locations also provides pharmacy-centered approach when developing policies and quality improvement projects at the system level.
Statistical analysis
The primary outcome measured was cost of drugs per statistic ($/day). Secondary outcomes included drug distribution, readmission rates, the number of pharmacy interventions, and safety measures including reduced turnaround time, BCMA, and medication errors (adjusted per 1,000 patient days). The transition success was analyzed for 2 years, pre- and post-implementation [2018–2022]. Financial data taken from each site-specific fiscal year (October 1st – September 30th) finance report was examined for drug expense per stat (dollars/days per month). Barcode scanning compliance data, defined as a percentage of drugs scanned, was procured from the EHR. Drug distribution data was obtained via ProDiver reporting. The medication error rate, defined as the number of serious safety events per 1,000 patient days, and readmission rates, defined as the number of patients readmitted to an acute-care setting, were reported on a monthly basis and obtained via the quality improvement scorecard documentation specific to each SNF and SNU location. The drug expense per patient, medication error rate, readmission rate, and number of pharmacist clinical inventions were non-parametric in nature and analyzed utilizing a Wilcoxon two-sample test. The software program utilized to analyze collected data was JMP Statistical Software (Cary, NC, USA). The BCMA data and distribution data were analyzed descriptively. An alpha value of P<0.05 was defined as statistically significant. Individualized patient data was not collected; instead, data was extracted from a deidentified Medicare quality report.
Results
Financial
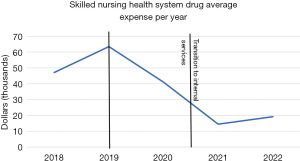
The SNF’s and SNU’s average monthly drug expense has decreased substantially following the transition to acute-care-based services. The primary outcome, average monthly drug expense per patient day ($/day), has decreased following the transition to acute-care-based services. Figure 3 displays the sum of drug expenses per month for the three skilled nursing locations. In January of 2019, a new SNF location was added, which contributed to an increased total drug expense. Total drug expenses were the highest from January 2019 to July 2020. During this time period, there were three skilled nursing facilities being cared for by vendor contracted pharmacists. Table 1 summarizes the drug costs before and after implementation, revealing a statistically significant difference (P<0.001). Prior to acute-care-based services, the median drug expense per day was $1,894.16 (806.29–2,401.63). Following implementation, the median drug expense was $544.77 (205.09–811.13). Overall, the total average drug expense for the three locations decreased by 71.2%. Figure 4 visualizes the sharp decline in average system drug expense following the conversion to acute-care-based services.
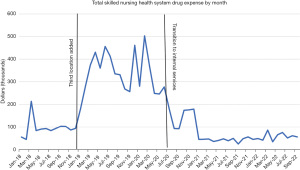
Table 1
| Outcome | Pre-implementation | Post-implementation | P value |
|---|---|---|---|
| Monthly drug expense per statistic ($/day) | 1,894.16 (806.29–2,401.63) | 544.77 (205.09–811.13) | <0.001 |
Data are shown as median (25–75% interquartile range).
Safety
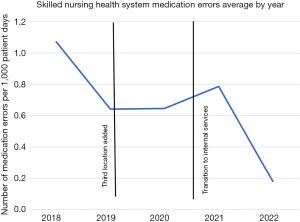
Prior to the transition in July 2020, BCMA was not utilized for medication administration. Therefore, the BCMA compliance rate was not available or zero. Figure 5 represents locational distinct SNU location’s BCMA compliance, respectively. Figure 6 represents the average BCMA compliance rate for the skilled nursing as a system. Since the implementation of the BCMA processes on a regular basis, all locations have met the 98% standard. Locations 1 and 2 have consistently exceeded the 98% compliance rate, while location 3 is typically in the 95–98% range. Three months following the transition, system BCMA compliance was consistently above the industry standard of 95% compliance. In August of 2020, the average system BCMA compliance rate had steadily increased to over 98%. Clearly, there has been a significant adoption of the BCMA system to deliver maximum patient safety benefits for our patients. Table 2 summarizes all secondary outcomes, includes medication errors/1,000 patient days. Medication errors were significantly reduced following implementation (P<0.001). Figure 7 displays the rate of medication errors as a negative linear slope. Adverse reactions were not specifically collected in our study. Instead, we focused on medication errors, specifically serious safety events adjusted per 1,000 patient days, as defined, and reported by Medicare. In the context of Medicare, a serious safety event is defined as an incident resulting in death, loss of a body part, disability, or a more than transient loss of a body function. It is important to note that this standardized definition remained consistent both before and after implementation, ensuring comparability of data.
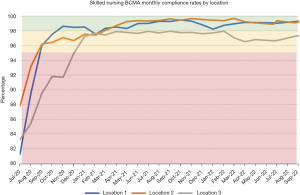
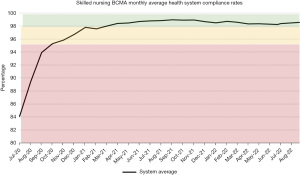
Table 2
| Outcome | Pre-implementation | Post-implementation | P value |
|---|---|---|---|
| Medication errors (/1,000 patient days) | 0.68 (0.08–2) | 0 (0–0.73) | <0.001 |
| Re-hospitalization rate (%) | 12.45 (10.4–14.62) | 15.2 (11.1–18.2) | 0.038 |
| Number of pharmacist interventions | 43.5 (24.24–56) | 149 (71–245) | <0.001 |
Data are shown as median (25–75% interquartile range).
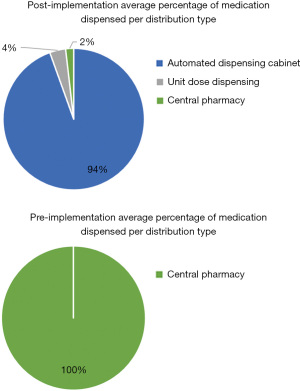
Distribution
Figure 8 displays the drug procurement processes from July 2020 to current for the SNF and SNU locations. Since July 2020, ADM’s have dispensed 94% of all doses dispensed within the SNF and SNU locations and 5.47% of medications were not contained within the ADM and required transport from an acute-care location located on or adjacent to the skilled nursing campus. Prior to July 2020, 100% of all patient medications were dispensed in blister pack format and delivered from a pharmacy located roughly two hours away from the facility. These deliveries were done twice daily, once in the morning around 5 AM and once in the evening between 8 and 9 PM. This ultimately left extended periods in which medication was not available or delayed for administration to the patient. Post implementation, the acute-care pharmacy sites transport medications at minimum three times a day to the designated skilled nursing location to refill the ADMs and deliver any new medications timely.
Clinical
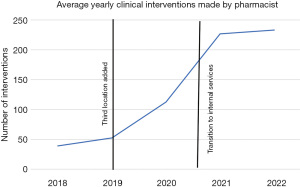
The number of pharmacist interventions was significantly increased, as displayed in Table 2 (P<0.001). The median number of pharmacist interventions prior to implementation was 43.5 (24.24–56), and the median number of pharmacist interventions following implementation was 149 [71–245]. Figure 9 outlines the clinical impact of the pharmacist within the SNF and SNU locations. Since 2018, clinical involvement by a pharmacist has increased by 242%, as measured by documented interventions.
Readmission
Return to acute rates significantly increased after the implementation of acute-care-based services. Table 2 outlines the median percentage of readmissions prior to 12.45% (10.4–14.62%) and post- 15.2% (11.1–18.2%) implementation (P=0.038).
Discussion
Key findings
Financial
Acute-care-based pharmacy services are associated with a decreased monthly drug expense.
Safety
The previous blister pack format was not optimal for use with the BCMA system. As a result, correct administration relied on a manual process of nurses matching patient to medication in a paper-based system, one of the many tasks conducted by an already busy nursing team. The transition was also associated with a decreased incidence of medication errors. An additional safeguard that contributed to a decrease in medication errors included an EHR that is synonymous with the acute-care EHR. Transcription of orders to paper introduces errors associated with incorrect transcription of medication name, dosage form, or strength. Transitioning to the computerized provider order entry system with pharmacist verification eliminated this step and associated errors.
Distribution
Medication turnaround time was considerably reduced from hours to minutes. ADMs can improve nurse access to medications, provide more efficient medication billing and inventory management, as well as increase medication security.
Clinical
The previous medication distribution system resulted in delays in medication administration, which could have adverse clinical effects specially when involving time critical and/or high-risk medications. Acute-care-based pharmacy services can streamline the admission process, as pharmacy staff provide continuous uninterrupted care and can verify orders at any given time. The dedicated clinical specialist performs comprehensive admission reconciliations, monthly medication and clinical reviews, and psychotropic medication reviews. The increased pharmacy footprint is displayed through the number of interventions made by a pharmacist. Most therapeutic interventions conducted by the pharmacists focused on two key drug classes: anticoagulants and antibiotics. These interventions were targeted at optimizing patient care and ensuring the appropriate use of these medications. Figure 10 outlines the percentage of patients that return to acute care following discharge to the skilled nursing on a quarterly basis. The pharmacist plays a crucial role in providing education to nursing staff regarding medication passes and bar code medication administration. Additionally, they actively engage with the nursing and provider teams on the floors, offering face-to-face visits to utilize their extensive drug expertise. The pharmacist also conducts one-on-one counseling sessions with nursing staff who may not be adhering to the BCMA standards. Furthermore, the clinical pharmacist performs audits to ensure compliance with accrediting body standards, including medication management. Moreover, the clinical specialist delivers monthly education sessions to providers and serves as a valuable resource daily for medication-related inquiries.

Strengths and limitations
There has been prior exploration as to whether acute-care-based SNF and SNU operations are clinically or financially beneficial. A potential limitation encountered was the absence of various historical data points, including clinical interventions made in 2018 in two locations. In addition, one location opened in 2019, limiting historical data for the entirety of the system (SNF and SNU). The rise of multiple variants of the coronavirus disease 2019 (COVID-19) virus was a major factor in skilled nursing patient readmissions in 2020 and 2021. This could skew the readmission data after 2020 in a positive direction.
Comparison with similar research
There is robust evidence that SNF patients can benefit greatly from the expertise of pharmacists. Through medication review, management, and counseling services, pharmacists can help optimize patient care delivery, ensure compliance with prescribed medications, and improve patient outcomes—all while reducing the associated medication cost to the health system. Despite the undeniable advantages of pharmacy services, there has yet to be a study that describes the best way to optimize these services between the two most popular options: an in-house pharmacy or a third-party vendor specialized in skilled nursing care.
Explanations of findings
Drug expense was reduced due to increased utilization of acute-care drugs at a better price, decreased waste, and the cessation of contracted service expenses. Drug waste decreased as the changes in therapy no longer resulted in the generation of a new blister pack. When the provider changed a dose, drug, or formulation, the blister pack format rendered all drugs contained within the pack unusable. The generation of a new blister pack was associated with the replacement of all of the drugs included in the patient’s regimen. In addition, the generation of a new blister pack restarted the medication procurement process and delayed therapy. Utilization of acute-care drugs allowed the health system to increase control over purchasing practices. Another factor in reduced drug expense was that previously medications were billed when dispensed, not administered. Under the acute care based system medications are billed upon administration to the specific patient, and retuned medications are eliminated.
Following the implementation of acute-care pharmacy-based services, BCMA became a top skilled nursing priority. Bar code medication initiation systems can provide real-time alerts when incorrect doses or medications are about to be administered, helping to prevent medication errors before they occur. The skilled nursing pharmacy clinical specialist led the BCMA initiative. Time was dedicated to the education of nursing staff and coaching nurses with low BCMA utilization rates. In addition to increasing safety, the use of BCMA and unit dose formats enables the patient to be charged on administration rather than dispensing, thus reducing medication waste and indirectly decreasing cost. The reduction in medication errors is multifactorial and includes the implementation of the BCMA system, a thorough clinical review performed by a dedicated pharmacist, and a decreased length of time associated with the procurement of the medication.
Medication administration by a facility located at or near the skilled nursing site ensures timely access to needed medications and timely patient care. The timely delivery of services facilitates the transition of care process and decreases the amount of time the health care team spends inquiring about medications. The use of ADMs decreases staff workload and allows individual doses to be dispensed immediately upon admission. Timely delivery of medications also increased provider flexibility and satisfaction by providing prescribers with the ability to immediately implement medication changes in therapy with great reduction in turnaround time. This data can also be integrated with the EHR system for improved accuracy and efficiency when selecting the medication prior to administration, minimizing risk of medication errors. The minimization of turnaround time is essential for ensuring that medications are administered in a timely manner and that patients receive the best possible care.
Readmission rates are impacted by the financial incentives associated with them by Medicare and other commercial health insurance plans (8). The reimbursement system in hospitals can motivate a health system to focus on discharging patients earlier. Under the prospective payment system, hospitals receive a fixed amount for each Medicare patient, regardless of the patient’s length of stay. Additionally, The COVID-19 pandemic began in March 2020, when the Secretary of the Department of Health and Human Services declared it a public health emergency. Cases began to spike as states eased social distancing restrictions in June 2020, leading to a large spike in U.S. cases over the winter months of 2020 (9). There is a possibility that healthcare costs were elevated due to readmissions of skilled nursing patients to the acute care setting, which was a concerning outcome in our study. However, in the subsequent discussion, we attributed this trend to factors such as the impact of COVID-19 and the dynamic nature of reimbursement models.
Implications and actions needed
Further research is needed to uncover the impact of acute-care pharmacy services on readmission rates and other clinical outcomes (ex: fall rates and hospital-acquired infections). The data provided by this study indicates health systems that have an integrated Skilled nursing site could demonstrate quality improvements and financially benefit from transitioning to their internal services. In addition, the increased pharmacy footprint provided by the internal service could reduce medication errors. Health systems should examine the feasibility of transitioning away from third-party services and maximizing their current pharmacy staff.
Conclusions
Utilizing existing internal pharmacy services for acute-care locations with affiliated SNFs and SNUs provides cost savings, improved safety outcomes, and increased clinical oversight. Though the data surrounding the optimization of services and readmission rates is limited, the associated financial and safety measures reported may lead other healthcare systems to consider optimizing the use of internal pharmacy services. Acute-care-based pharmacy services can be associated with a decrease in monthly drug expenses due to decreased waste, cessation of contracted services, and increased control over purchasing practices. The use of BCMA systems and unit-dose formats also increased safety by providing real-time alerts and decreasing medication errors. Medication turnaround time was decreased from hours to minutes, and the transition was associated with a decrease in medication errors due to the use of an EHR system. The COVID-19 pandemic has led to an increase in skilled nursing patient readmissions due to financial incentives for hospitals to discharge patients earlier. Decreasing length of stay while decreasing readmissions has become a dual focus for hospitals, and pharmacists can play a significant role in achieving these goals when integrated into the care team in any practice setting.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-27/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-27/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-27/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rough S, Shane R, Armitstead JA, et al. The high-value pharmacy enterprise framework: Advancing pharmacy practice in health systems through a consensus-based, strategic approach. Am J Health Syst Pharm 2021;78:498-510. [Crossref] [PubMed]
- Lee SWH, Mak VSL, Tang YW. Pharmacist services in nursing homes: A systematic review and meta-analysis. Br J Clin Pharmacol 2019;85:2668-88. [Crossref] [PubMed]
- Christensen D, Trygstad T, Sullivan R, et al. A pharmacy management intervention for optimizing drug therapy for nursing home patients. Am J Geriatr Pharmacother 2004;2:248-56. [Crossref] [PubMed]
- Achilleos M, McEwen J, Hoesly M, et al. Pharmacist-led program to improve transitions from acute care to skilled nursing facility care. Am J Health Syst Pharm 2020;77:979-84. [Crossref] [PubMed]
- Standards of Practice for Clinical Pharmacists. [cited 2023 Jun 26]. Available online: https://www.accp.com/docs/positions/guidelines/standardsofpractice.pdf
- Tong EY, Edwards G, Hua PU, et al. Systematic review of clinical outcomes of clinical pharmacist roles in hospitalized general medicine patients. J Pharm Pract Res 2020;50:297-307. [Crossref]
- Kaboli PJ, Hoth AB, McClimon BJ, et al. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med 2006;166:955-64. [Crossref] [PubMed]
- Upadhyay S, Stephenson AL, Smith DG. Readmission Rates and Their Impact on Hospital Financial Performance: A Study of Washington Hospitals. Inquiry 2019;56:46958019860386. [Crossref] [PubMed]
- CDC Museum Covid-19 Timeline [Internet]. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention; 2022 [cited 2023 Jan 20]. Available online: https://www.cdc.gov/museum/timeline/covid19.html#:~:text=January%2031%2C%202020&text=The%20Secretary%20of%20the%20Department,outbreak%20a%20public%20health%20emergency
Cite this article as: Vanderlee A, Armitstead JA, Darnell J, Lozano Y. Impact of acute-care pharmacy services on health system skilled nursing locations. J Hosp Manag Health Policy 2023;7:13.

