
Financial performance of rural hospitals persistently lacking or having telehealth technology
Highlight box
Key findings
• Using longitudinal data over an 11-year study period, rural hospitals that persistently lacked telehealth services had severe financial problems.
• Rural hospitals persistently lacking telehealth services resided in areas with a greater need for telehealth service as evidenced by having less dense populations in poorer communities with less health insurance.
What is known and what is new?
• Rural hospitals struggle financially, limiting their ability to provide necessary services including telehealth options.
• This manuscript identifies hospitals with severe financial issues that persistently lacked telehealth technology despite being in areas that may benefit significantly from having the technology.
What is the implication, and what should change now?
• Rural hospitals with the best potential to improve health due to being in poorer, less dense areas are least able to afford telehealth technology.
• Policies are needed to enable hospitals in the poorest communities to provide telehealth services.
Introduction
Background
Rural hospitals, defined as short-term, general acute, nonfederal facilities with special payment designations (Critical Access Hospital, Medicare Dependent Hospital, Sole Community Hospital, and Rural Referral Center), as well as other hospitals located in counties or sub-county areas with a Rural-Urban Commuting Area (RUCA) code of 4 or greater, struggle with maintaining operations in the current healthcare environment. Common challenges include low reimbursement rates, sicker patients, remote geographical locations, older and poorer patients, health professional shortages, shrinking rural populations, and increased travel distances for patients (1,2). These challenges create financial pressures for rural hospitals and threaten their ability to provide accessible quality healthcare services. To mitigate these challenges, some rural hospitals have adopted telehealth technology (3,4). In this study, telehealth is defined as “a broad variety of technologies and tactics to deliver virtual medical, public health, health education delivery, and support services using telecommunications technologies (5).” Telehealth can decrease healthcare costs while improving access to specialty services, allowing rural patients to remain in the community, and reducing rural provider burnout (6). Despite the benefits of telemedicine to populations served by hospitals, variation exists in telehealth adoption among rural hospitals.
Telehealth adoption by rural hospitals is multifaceted, influenced by hospitals’ financial conditions, and intertwined with hospital and community characteristics (7). Financially well-off rural hospitals with high operating and total margins may be more likely to adopt telehealth compared to financially disadvantaged rural hospitals due to the burden of up-front capital investment (3). Financial barriers thus may explain part of the observed disparities in telehealth adoption by rural hospitals (2).
Rationale and knowledge gap
Many studies have examined the benefits of telehealth adoption on patient outcomes, quality, and access (6-8). Several prior studies examined the overall cost of telehealth services; however, most of those studies compare the cost of a telehealth service relative to a comparable in-person service in a single healthcare setting (9,10) or examine hospital financial performance using claims that cannot be linked to specific hospitals (11). One additional study used qualitative interviews with rural hospital Chief Financial Officers across 10 states (12), and another examined telehealth costs using a national sample but examined direct costs to consumers rather than hospital financial performance (13).
Objective
The purpose of this study is to compare the operating and total margins of rural hospital telehealth adopters (persistently reported telehealth use over the 11-year study period) and non-adopters (no evidence of telehealth over the study period) and evaluate factors associated with telehealth adoption and the relationship between telehealth adoption and financial margins. The primary hypothesis was that rural hospitals that persistently lacked telemedicine over the study were in worse financial shape than adopters. Both hospital and community characteristics were also assessed to explain the financial obstacles that hinder rural hospital telehealth adoption. We present this article in accordance with the STROBE reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-85/rc).
Methods
Study sample
This study used retrospective longitudinal cohort study designed to examine differences in rural hospital characteristics, especially profitability, and telehealth adoption from 2009 to 2019. Data were obtained from the American Hospital Association (AHA) Annual Survey and Information Technology (IT) supplement, the Centers for Medicare & Medicaid Services (CMS) Hospital Cost Report Information System, and the Area Health Resource File (AHRF). These datasets provide detailed information on hospital characteristics, telehealth status, hospital financial performance, and county-level characteristics. The cost report data were merged by the hospital, while the AHRF was merged by county.
The study sample was a longitudinal, unbalanced panel consisting of rural hospitals persistently with or without telehealth adoption. Telehealth adoption status was determined using the AHA IT Supplement and included rural hospitals that had outpatient or inpatient telehealth services for the entire study period. Due to longitudinal survey variability, telehealth adoption status was collapsed into a dichotomous variable (adopters versus non-adopters) by year. Rural hospitals persistently identified as telehealth adopters during the study period were designated as “Telehealth Adopters”; rural hospitals persistently identified as telehealth non-adopters were designated as “Telehealth Non-Adopters”. The final sample consisted of 600 rural hospitals (2,675 rural hospital-year observations) of which 325 were adopters and 275 were non-adopters, representing approximately 25 percent of all rural hospitals in the United States (U.S.).
Study variables
Since rural hospital telehealth adoption is associated with the financial, hospital, and community factors, we compared differences in these variables between Telehealth Adopters and Telehealth Non-Adopters. Hospital characteristics include structural factors and processes that may influence operations, strategy, and revenue generation (14). Hospital characteristics included whether the hospital was government-owned, not-for-profit, or for-profit, bed size, and information on the payer mix (percent hospitalizations paid by the state/federal Medicaid program and federal Medicare program). The U.S. Medicare program provides health insurance to all adults aged 65 and over who elect it. Part A of Medicare covers hospital care and financing rules within the program can have important consequences for hospital profitability. During the study period, the Medicare program allowed reimbursement for telehealth services in rural areas only.
Community characteristics describe the hospital’s operating environment and market demand for health services (15). Community characteristics based on the county of the hospital included population density, the percent of the county population over 65 (and thus eligible for Medicare), the county unemployment rate, the percentage of people lacking any form of health insurance, the median per capita income, the poverty rate, and a measure of concentration based on the number of hospitals in the county.
Financial performance was measured using both hospital operating margins and total margins. Operating margin [(operating revenues − expenses)/operating revenues] is a measure of profitability from hospital operations. Total margin [(total revenues − expenses)/total revenues] is a measure of overall profitability and income from both operating and non-operating sources. Profitability is an indicator of a hospital’s ability to both generate revenue and manage costs (16).
Statistical analysis
We conducted bivariate analyses to test for differences between subgroup means of Telehealth Adopters and Telehealth Non-Adopters using t-tests for continuous variables and chi-square tests for categorical variables using α≤0.05. Multivariate analysis was accomplished by a logistic regression model to evaluate the association of hospital and community characteristics with rural hospital telehealth adoption and an ordinary least squares (OLS) regression with robust standard errors to assess the association of rural hospital telehealth adoption on hospital financial performance (operating margin and total margin), controlling for hospital and community characteristics. The logistic regression was chosen because of the dichotomous dependent variable. The OLS regression was chosen without transformation as there was no evidence of skewness in the descriptive analysis of the operating and total margin variables. Results from both regressions are reported as average marginal effects. All statistical analyses were completed using STATA 17.0 (17).
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study did not require written inform consent and approval by the institutional/regional/national ethics/committee ethics board, because all the data were retrieved from datasets.
Results
By comparing the profitability of rural hospital Telehealth Adopters and rural hospital Telehealth Non-Adopters over the period between 2009 and 2019, we determined financial health is associated with telehealth adoption. Figure 1 displays the average annual operating margin for rural hospital Telehealth Adopters and Non-Adopters. The average annual operating margin for Telehealth Adopters remained positive across all years of the study period, except for the first year, averaging 1.49%. In contrast, the Telehealth Non-Adopters consistently experienced negative average annual operating margins over the entire study period averaging −7.73%. Figure 2 displays the annual average total margin for Telehealth Adopters and Telehealth Non-Adopters in rural hospitals. The average total margin was higher for Telehealth Adopters (4.14%) compared to Telehealth Non-Adopters (1.35%).
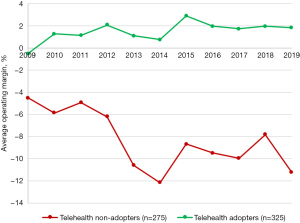
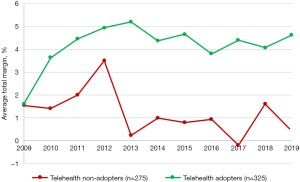
Figure 3 provides a similar analysis with hospital operating margins broken out by ownership status. Government hospitals that were non-adopters had the lowest operating margin of any hospital type in either category with average returns between −10 and −15 percent. For-profit hospitals that were adopters had the highest operating margin with returns averaging 5 percent. For-profit non-adopters and not-for-profit non-adopters both had average margins that exceeded operating margins for government hospitals that adopted.
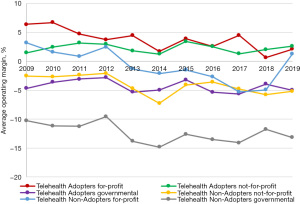
Figure 4 shows total margins by hospital ownership status and illustrates higher returns for telehealth-adopting hospitals relative to non-adopting hospitals. In general, both for-profit and not-for-profit hospitals that adopted telehealth had higher margins relative to non-adopting hospitals. Even the total margins for government hospitals were higher on average relative to non-adopting hospitals.
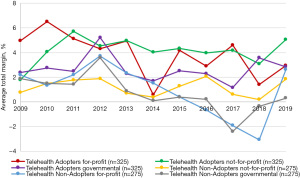
Table 1 provides descriptive statistics for all rural hospitals stratified by Telehealth Adopters and Telehealth Non-Adopters status. Hospital profitability was significantly different between the two rural hospital categories. Both the average operating margin and total margin for rural Telehealth Adopters were greater (1.49% and 4.14%, respectively) than the rural Telehealth Non-Adopters (−7.73% and 1.35%, respectively).
Table 1
| Variables | All rural hospitals (n=2,675 hospital-year observations from 600 hospitals) | Telehealth Adopters (n=1,677 hospital-year observations from 325 hospitals) |
Telehealth Non-Adopters (n=998 hospital-year observations from 275 hospitals) | P value |
|---|---|---|---|---|
| Financial performance | ||||
| Operating margin (×100) | −1.95 (13.84) | 1.49 (10.26) | −7.73 (16.84) | <0.001 |
| Total margin (×100) | 3.10 (9.78) | 4.14 (9.20) | 1.35 (10.45) | <0.001 |
| Hospital characteristics | ||||
| Ownership status | <0.001 | |||
| Not-profit hospitals | 1,476 [55.18] | 1,090 [65.00] | 386 [38.68] | |
| Government hospitals | 844 [31.55] | 400 [23.85] | 444 [44.49] | |
| For-profit hospitals | 355 [13.27] | 187 [11.15] | 168 [16.83] | |
| Total beds | 120.06 (207.30) | 151.53 (239.09) | 67.18 (121.21) | <0.001 |
| Medicare payer mix percentage | 48.56 (15.98) | 46.25 (14.58) | 52.44 (17.42) | <0.001 |
| Medicaid payer mix percentage | 10.68 (9.27) | 10.89 (8.91) | 10.32 (9.82) | 0.121 |
| Community characteristics | ||||
| Population density (persons per square mile) | 458.17 (4,462.49) | 547.32 (5,248.73) | 308.36 (2,657.54) | 0.181 |
| Percent seniors (≥65 years) | 17.43 (4.03) | 17.51 (3.89) | 17.30 (4.25) | 0.204 |
| Unemployment rate (%) | 6.66 (3.17) | 6.41(3.15) | 7.07 (3.15) | <0.001 |
| Percent <65 years without health insurance | 14.73 (5.99) | 13.60 (5.38) | 16.62 (6.46) | <0.001 |
| Per capita income ($) | 39,977.12 (12,885.24) | 41,181.73 (13,945.39) | 37,952.94 (10,575.30) | <0.001 |
| Poverty rate (%) | 16.23 (5.76) | 15.79 (5.50) | 16.96 (6.10) | <0.001 |
| Hospital concentration (# of hospitals in the county) | 2.81 (6.62) | 3.13 (7.92) | 2.27 (3.45) | 0.0011 |
| Year variables | <0.001 | |||
| 2009 | 321 [12.00] | 159 [9.48] | 162 [16.23] | |
| 2010 | 266 [9.94] | 146 [8.71] | 120 [12.02] | |
| 2011 | 237 [8.86] | 142 [8.47] | 95 [9.52] | |
| 2012 | 260 [9.72] | 154 [9.18] | 106 [10.62] | |
| 2013 | 218 [8.15] | 133 [7.93] | 85 [8.52] | |
| 2014 | 225 [8.41] | 137 [8.17] | 88 [8.82] | |
| 2015 | 233 [8.71] | 148 [8.83] | 85 [8.52] | |
| 2016 | 237 [8.86] | 165 [9.84] | 72 [7.21] | |
| 2017 | 222 [8.30] | 162 [9.66] | 60 [6.01] | |
| 2018 | 235 [8.79] | 166 [9.90] | 69 [6.91] | |
| 2019 | 221 [8.26] | 165 [9.84] | 56 [5.61] | |
Data are presented as mean (SD) or n [%]. Telehealth Adopter hospitals are defined as rural hospitals that have continuously adopted telehealth and Telehealth Non-Adopters hospitals are defined as rural hospitals that have never adopted telehealth.
Hospital characteristics differed significantly between rural hospital Telehealth Adopters and Telehealth Non-Adopters. Compared to Telehealth Non-Adopters, Telehealth Adopters were largely not-for-profit (65.00%), had larger facilities (151.53 versus 67.18 average total beds), and served a lower percentage of Medicare patients (46.25% versus 52.44% average Medicare payer mix). Community characteristics also differed across the two groups. Telehealth Adopters were physically located in counties with higher population density (547.32 versus 308.36 persons per square mile), higher income ($41,181.73 versus $37,952.94 per person), and more hospitals (3.13 versus 2.27 hospitals). Telehealth Non-Adopters were physically located in counties with higher unemployment rates (7.07% versus 6.41%), a higher percentage of people <65 years without health insurance (16.62% versus 13.60%), and higher poverty rates (16.96% versus 15.79%).
Table 2 provides the logistic regression results estimating the likelihood the rural hospital is a Telehealth Adopter. Both for-profit and government hospitals had a significantly lower probability to be designated a rural Telehealth Adopter hospital by 16 and 17 percentage points, respectively. An increase in the Medicare payer mix was associated with a significantly lower probability to be designated a rural hospital Telehealth Adopter. An increase in either population density or percentage of people <65 years without health insurance was associated with a significantly lower probability to be designated a rural hospital Telehealth Adopter. However, an increase in hospital concentration (number of hospitals in the county) was associated with a significantly higher probability to be categorized as a rural hospital Telehealth Adopter.
Table 2
| Independent variables | Telehealth status: Adopters versus Non-Adopters | |
|---|---|---|
| Marginal effects (dy/dx) | Standard errors | |
| Hospital characteristics | ||
| Government hospitals† | −0.17*** | 0.021 |
| For-profit hospitals† | −0.16*** | 0.029 |
| Total beds | 0.00060*** | 0.00010 |
| Medicare payer mix percentage | −0.0037*** | 0.00070 |
| Medicaid payer mix percentage | −0.000094 | 0.0011 |
| Community characteristics | ||
| Population density (persons per square mile)‡ | −0.020* | 0.0086 |
| Percent seniors (≥65 years) | 0.0046 | 0.0026 |
| Unemployment rate (%) | 0.00073 | 0.0042 |
| Percent <65 years without health insurance | −0.013*** | 0.0021 |
| Per capita income ($)‡ | −0.072 | 0.058 |
| Poverty rate (%) | −0.0019 | 0.0023 |
| Hospital concentration (# of hospitals in the county) | 0.0042* | 0.0016 |
| Year variables | ||
| 2009 (ref) | − | − |
| 2010 | 0.043 | 0.038 |
| 2011 | 0.090* | 0.039 |
| 2012 | 0.072 | 0.038 |
| 2013 | 0.084* | 0.041 |
| 2014 | 0.059 | 0.043 |
| 2015 | 0.042 | 0.045 |
| 2016 | 0.084 | 0.046 |
| 2017 | 0.130** | 0.047 |
| 2018 | 0.100* | 0.047 |
| 2019 | 0.140** | 0.048 |
The logistic regression model helps to identify the hospital and community factors that contribute to becoming a Telehealth Adopters versus a Telehealth Non-Adopters hospital. *, P<0.05; **, P<0.01; ***, P<0.001. †, referent is not-for-profit hospitals; ‡, natural log-transformed variable.
Table 3 presents results from the pooled OLS regression. The regression estimates the association of operating and total margin as a function of rural hospital telehealth adoption (Telehealth Adopters versus Telehealth Non-Adopters), controlling for hospital attributes, community characteristics, and time dummy variables. During the study period, Telehealth Adopters experienced a significant increase in both operating margin (6.92 percentage points, P<0.001) and total margin (2.18 percentage points, P<0.001) compared to Telehealth Non-Adopters. In comparison to not-for-profit hospitals, government hospitals were associated with a significant decrease in operating margin, whereas for-profits were associated with a significant increase in operating margin. An increase in the percent seniors, those <65 years without health insurance, per capita income, and poverty rate all had a significant negative effect on operating margin. A similar relationship was found with total margin, except per capita income, which had a significant positive effect on total margin. After controlling for both hospital and community characteristics, there were no significant trends in either operating or total margin over time.
Table 3
| Independent variables | Operating margin (%) | Total margin (%) | |||
|---|---|---|---|---|---|
| Marginal effects (dy/dx) | Robust standard errors | Marginal effects (dy/dx) | Robust standard errors | ||
| Hospital telehealth status† | 6.92*** | 0.54 | 2.18*** | 0.41 | |
| Hospital characteristics | |||||
| Government hospitals‡ | −4.48*** | 0.56 | −0.30 | 0.40 | |
| For-profit hospitals‡ | 3.39*** | 0.81 | 0.46 | 0.70 | |
| Total beds | 0.0025 | 0.0014 | 0.0033** | 0.0011 | |
| Medicare payer mix percentage | −0.019 | 0.022 | −0.058*** | 0.016 | |
| Medicaid payer mix percentage | 0.160*** | 0.032 | −0.055** | 0.024 | |
| Community characteristics | |||||
| Population density (persons per square mile)§ | 0.19 | 0.25 | −0.49** | 0.18 | |
| Percent seniors (≥65 years) | −0.39*** | 0.079 | −0.34*** | 0.063 | |
| Unemployment rate (%) | 0.130 | 0.110 | −0.040 | 0.087 | |
| Percent <65 years without health insurance | −0.55*** | 0.076 | −0.0087 | 0.049 | |
| Per capita income ($)§ | −5.26** | 1.84 | 2.71* | 1.27 | |
| Poverty rate (%) | −0.170* | 0.070 | −0.068 | 0.054 | |
| Hospital concentration (# of hospitals in the county) | −0.044 | 0.030 | −0.040* | 0.019 | |
| Year variables | |||||
| 2009 (ref) | − | − | − | − | |
| 2010 | 0.097 | 0.94 | 0.74 | 0.74 | |
| 2011 | 0.64 | 1.04 | 1.35 | 0.79 | |
| 2012 | 0.99 | 1.04 | 2.27** | 0.78 | |
| 2013 | −1.02 | 1.17 | 1.13 | 0.92 | |
| 2014 | −2.86* | 1.27 | 0.75 | 0.97 | |
| 2015 | −1.57 | 1.25 | 1.02 | 0.98 | |
| 2016 | −2.48 | 1.34 | 0.56 | 0.96 | |
| 2017 | −1.89 | 1.37 | 0.48 | 1.03 | |
| 2018 | −0.82 | 1.34 | 0.82 | 1.05 | |
| 2019 | −0.98 | 1.36 | 0.77 | 1.06 | |
The ordinary least squares regression model helps to assess the relationship between profitability and Telehealth Adopters and Telehealth Non-Adopters status, controlling for hospital and community characteristics. *, P<0.05; **, P<0.01; ***, P<0.001. †, referent is hospital telehealth status (no telehealth, i.e., Telehealth Non-Adopters); ‡, referent is not-for-profit hospitals; §, natural log-transformed variable.
Discussion
Key findings
The study analysis finds that a large number of rural hospitals never implemented telehealth (non-adopters) over the study period. The non-adopters report much worse financial performance relative to hospitals that always had telehealth services (telehealth adopters). The study also provides evidence on how hospital financial conditions and hospital and community characteristics are associated with telehealth adoption.
Strengths and limitations
There were several limitations associated with this study. First, the main limitation of this study is differentiating the levels of telehealth adoption. Due to inconsistencies in telehealth definitions utilized over time and variations in the degree of telehealth adoption, we are unable to determine the association between the extent of rural hospital telehealth adoption and financial performance. It is possible that some of the adopters had limited capabilities associated with telehealth. Second, there is an inherent limitation with using administrative secondary data, which includes data errors, missing data, and the retrospective nature of data collection. It should be noted that administrative secondary data are not typically collected for research purposes or to test specific hypotheses. Despite these limitations, we hope that the results of this study highlight the relationship between rural hospitals’ financial condition and prioritizing capital investment decisions. Third, the study focused on a definition of persistence to identify a clear demarcation of hospital types. The subset of hospitals in this study was therefore not representative of all rural hospitals, but instead, limited to hospitals defined by their persistent use or non-use of telehealth. Finally, our interest was in understanding the financial factors associated with adoption. Numerous other outcomes could be studied that may differ between persistent adopters and non-adopters including measures of quality, community outcomes, and treatment costs among others. A case can be made for addressing these outcomes in future research.
Comparison with similar research
It is important to note that the coronavirus disease 2019 (COVID-19) pandemic changed telehealth adoption, which became the primary means of providing healthcare for many rural hospitals. The unplanned investment put existing financially vulnerable rural hospitals in a precarious position. Reduced patient revenues and dwindling funds created challenges for some rural hospitals as they navigated the uncertainty of the pandemic. Telehealth adoption, which started as a temporary fix for rural hospitals to ensure healthcare access during the pandemic, maybe a good long-term investment for struggling rural hospitals. Federal investment into telehealth during the pandemic increased greatly and we expect will allow many of the non-adopting hospitals to obtain telehealth. An evaluation of the change in adoption status in 2020 is an important area for research. In addition, a causal analysis of the financial impact of telehealth adoption has not been conducted and may reveal new insights, especially during the pandemic. It is important to recognize that reimbursement changes, patient retention, and reduced hospital staffing costs, among others, may contribute to improving hospital financial performance (6) and these were not addressed in the current analysis.
Explanations of findings
The results from this study confirm that differences in telehealth adoption exist among rural hospitals, especially in terms of financial performance. The large difference in financial performance between the Telehealth Adopters and Non-Adopters was unexpected and suggests that Telehealth Non-Adopters may not be able to allocate the funding capital to become Telehealth Adopters without policies or monetary support to finance this type of investment. The absence of telehealth adoption in rural hospitals also means that patients may not have the option to receive needed care and may be expected to travel to other community hospitals for care (18). The disparity in telehealth services creates serious equity concerns and has implications for patient access, quality, and outcomes for rural patients.
Implications and actions needed
Rural hospital financial well-being was significantly related to telehealth adoption. Higher profit margins were observed by the Telehealth Adopters compared to the Telehealth Non-Adopters from 2009 to 2019, supporting an association between rural hospital financial health and telehealth adoption. While these results confirm a correlation between financial health and telehealth adoption, they do not imply causation, i.e., telehealth adoption does not necessarily improve rural hospital financial health, or vice versa. Additional research is needed to determine causal relationships between hospital financial health and telehealth adoption among rural and urban hospitals.
Conclusions
Unprofitable rural hospitals face endless financial hardships, which may explain the absence of telehealth adoption by some hospitals. The capital investment, operating costs, reduced patient demand, and low reimbursement associated with telehealth care delivery make it difficult to prioritize investment into telehealth adoption (19). Our findings demonstrate that rural hospitals with the best potential to improve health due to being in poorer, less dense areas, may be the least likely to afford telehealth technology, which adversely impacts their ability to deliver services to their rural residents. Unlike impoverished rural hospitals, well-to-do rural hospitals can invest in telehealth infrastructure to improve patient care delivery (20). The large financial inequality reported here demonstrates severe inequity among rural hospitals compromising healthcare access for rural patients.
Acknowledgments
Funding: This study received funding from the Office for the Advancement of Telehealth and the US Health Resources and Services Administration Grant #U3GRH40001 to conduct evaluation research on telehealth services, which aligns with Section 711 of the Social Security Act.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-85/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-85/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-85/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-85/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study did not require written inform consent and approval by the institutional/regional/national ethics/committee ethics board, because all the data were retrieved from datasets.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bai G, Yehia F, Chen W, et al. Varying Trends In The Financial Viability Of US Rural Hospitals, 2011-17. Health Aff (Millwood) 2020;39:942-8. [Crossref] [PubMed]
- Murphy KM, Hughes LS, Conway P. A Path to Sustain Rural Hospitals. JAMA 2018;319:1193-4. [Crossref] [PubMed]
- Banbury A, Smith AC, Mehrotra A, et al. A comparison study between metropolitan and rural hospital-based telehealth activity to inform adoption and expansion. J Telemed Telecare 2023;29:540-51. [Crossref] [PubMed]
- Gaziel-Yablowitz M, Bates DW, Levine DM. Telehealth in US hospitals: State-level reimbursement policies no longer influence adoption rates. Int J Med Inform 2021;153:104540. [Crossref] [PubMed]
- Fact Sheet: Telehealth | AHA [Internet]. [cited Apr 16, 2023]. Available online: https://www.aha.org/factsheet/telehealth
- Telehealth Use in Rural Healthcare Overview - Rural Health Information Hub [Internet]. RHIhub Rural Health Information Hub. 2021 [cited 2022 Apr 29]. Available from: https://www.ruralhealthinfo.org/topics/telehealth#financial-impact
- Chen J, Amaize A, Barath D. Evaluating Telehealth Adoption and Related Barriers Among Hospitals Located in Rural and Urban Areas. J Rural Health 2021;37:801-11. [Crossref] [PubMed]
- Gajarawala SN, Pelkowski JN. Telehealth Benefits and Barriers. J Nurse Pract 2021;17:218-21. [Crossref] [PubMed]
- Williams D Jr, Simpson AN, King K, et al. Do Hospitals Providing Telehealth in Emergency Departments Have Lower Emergency Department Costs? Telemed J E Health 2021;27:1011-20. [Crossref] [PubMed]
- Bassin BS, Haas NL, Sefa N, et al. Cost-effectiveness of an Emergency Department-Based Intensive Care Unit. JAMA Netw Open 2022;5:e2233649. [Crossref] [PubMed]
- Cornaggia K, Li X, Ye Z. Financial Effects of Remote Product Delivery: Evidence from Hospitals [Internet]. Rochester, NY; 2023 [cited Jun 15, 2023]. Available online: https://papers.ssrn.com/abstract=3833193
- Uscher-Pines L, Sousa JL, Zachrison KS, et al. Financial impact of telehealth: rural chief financial officer perspectives. Am J Manag Care 2022;28:e436-43. [Crossref] [PubMed]
- Tak HJ, Cozad M, Horner RD. A National Perspective of Telemedicine Use and Direct Medical Costs: Who Uses It and How Much It Costs. Med Care 2023;61:495-504. [Crossref] [PubMed]
- Nedelea IC, Fannin JM, editors. Efficiency Analysis of Rural Hospitals: Parametric and Semi-parametric Approaches. AgEcon Search; 2012:1-19.
- Kaufman BG, Thomas SR, Randolph RK, et al. The Rising Rate of Rural Hospital Closures. J Rural Health 2016;32:35-43. [Crossref] [PubMed]
- Gapenski LC, Vogel WB, Langland-Orban B. The determinants of hospital profitability. Hosp Health Serv Adm 1993;38:63-80. [PubMed]
- Stata 17.
0. 2021. Available online: https://www.stata.com/ - Anthony B Jnr. Implications of telehealth and digital care solutions during COVID-19 pandemic: a qualitative literature review. Inform Health Soc Care 2021;46:68-83. [Crossref] [PubMed]
- Puro NA, Feyereisen S. Telehealth Availability in US Hospitals in the Face of the COVID-19 Pandemic. J Rural Health 2020;36:577-83. [Crossref] [PubMed]
- Zachrison KS, Richard JV, Mehrotra A. Paying for Telemedicine in Smaller Rural Hospitals: Extending the Technology to Those Who Benefit Most. JAMA Health Forum 2021;2:e211570. [Crossref] [PubMed]
Cite this article as: Karim SA, Tilford JM, Bogulski CA, Rabbani M, Hayes CJ, Eswaran H. Financial performance of rural hospitals persistently lacking or having telehealth technology. J Hosp Manag Health Policy 2023;7:9.

