Strategies for enriching the resident, fellow, and faculty physician experience: a system-based approach to physician well-being
Introduction
Physician burnout crisis
Physician burnout and psychological distress have been increasingly recognized as a public health crisis (1). While a national survey demonstrated that the prevalence of physician burnout in 2020 was lower than prior years, physicians are still at approximately 40% higher risk of burnout when compared to the general working population (2). In a meta-analysis of over 20 survey studies, graduate medical education (GME) trainees (residents and fellows) reported a cross-specialty overall burnout prevalence of over 35% (3). A number of studies have suggested several drivers of physician burnout, including excessive clerical work, lack of sleep, longer work hours, and an imbalance between occupational demands and resources (4,5). In our own work, we found that clinical faculty who report spending >90 min/day on the electronic health record (EHR) after work had an almost two-fold increased likelihood of burnout, and those who report spending >60 min/day on clerical tasks had a 1.4 increased risk for experiencing work-related stress (6).
Aside from the moral imperative to address a workforce suffering from these outcomes, physician burnout has been shown to negatively affect the delivery of healthcare by contributing to decreased quality of care, medical errors, poor patient satisfaction, and an increased cost of physician turnover and productivity (7,8). Systems-directed well-being initiatives have been demonstrated to be equally effective, and likely superior to, individual-level programming (9-11). Examples of systems-level initiatives include medical documentation scribes, enhanced or expanded team-based care models, schedule modifications, EHR optimization, and utilization of quality improvement strategies to improve workflows, all of which have been shown to either decrease burnout and stress and/or increase professional satisfaction (12).
Background: our response to physician burnout
Beginning in 2017, leading healthcare organizations began creating Chief Wellness Officer (CWO) positions to guide the organizational well-being strategy and cultural transformation needed to reduce burnout among physicians (13). Our own Mount Sinai Health System (MSHS) formed the Office of Well-Being and Resilience (OWBR) in 2018, sitting within the Icahn School of Medicine at Mount Sinai (ISMMS) and led by a CWO. The OWBR mission seeks to “promote your well-being and professional satisfaction by advancing a culture that enables you to do your best work in a community that values you.” As the OWBR sits in the Office of the Dean of the medical school, the constituents of the program at our institution include the faculty of the medical school (physicians and scientists), GME trainees (residents and fellows), medical students and biomedical science graduate students and post-doctoral fellows. To address the needs of each of these groups, there is an Associate Dean for each constituency. The Associate Deans create infrastructure and programming to assess and improve the well-being of their constituent groups. The OWBR staff also includes a director, mental health liaison, program coordinator, administrative assistant, associate researcher, clinical research coordinator and a scholarly year medical student. In this paper, we will focus on the 2 clinical constituent groups under the OWBR’s charge—faculty physicians and GME trainees.
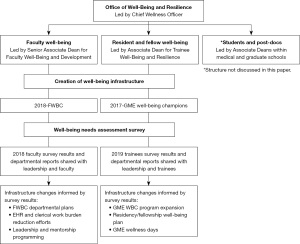
Under the leadership of the Associate Deans of GME Trainee and Faculty Well-Being and to improve the well-being of our physician cohorts (faculty, residents, and fellows), we implemented a three-pronged approach: (I) creating infrastructure to promote well-being via our Well-Being Champion Program; (II) distributing and analyzing needs assessment surveys; and (III) utilizing the infrastructure and survey results to implement interventions targeting the drivers of burnout and stress. Figure 1 outlines a workflow that summarizes this approach. In this paper, we aim to describe how our infrastructure and needs assessment surveys for both cohorts impacted the development of interventions to improve well-being for faculty and trainee physicians. We report data from the 2018–2019 faculty survey and 2019 graduate medical trainee survey that were used to further create and enhance well-being programs and interventions.
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of the Icahn School of Medicine at Mount Sinai (No. 18-01090 for faculty survey, 17-02885 for graduate medical education survey) and individual consent for this retrospective analysis was waived.
Setting and participants
Our program needs assessment and interventions occur across the Mount Sinai Health System, a large urban health care system in NYC (New York City), with eight hospitals and a large ambulatory care footprint across four Boroughs and Long Island. Employed faculty, residents, and fellows in the healthcare system are included in this program.
Program development and description: Well-Being Champions (WBC)
Distinct Faculty and GME WBC programs were created given the size and complexity of our institution which leads to variable needs among physicians and GME trainees within different specialties and across practice sites. As such, we aim to have expert ambassadors with a “boots on the ground” perspective to help move the work forward. The WBC programs aim to engage faculty in each department and advocate for efforts to promote the well-being of their department-level constituents (faculty and/or GME trainees).
Faculty Well-Being Champion (FWBC) program
Overseen by the Associate Dean for Faculty Well-Being, the FWBC program was developed in 2018 (just prior to our first faculty survey administration) to better understand the well-being needs of faculty and to begin to improve well-being at the departmental level. Since drivers of well-being and professional fulfillment are complex and vary by clinical site, specialty, and years in practice, we sought to create a learning community of well-being leaders in all clinical departments across the Mount Sinai Health System (MSHS). The group shares challenges and barriers, explores best practices, serves as the collection of local experts knowledgeable of existing MSHS support resources, and functions as a supportive network. To recruit faculty members into this role, the CWO and the Associate Dean met with the chairpersons from each department to gain buy-in and commitment (with the support of the Dean of the Medical School) for this program. Each chairperson was then asked to appoint one or more faculty members to the role of FWBC for their department. Appropriate candidates for this role are faculty peers who are well-respected by both their colleagues and their leaders and have the leadership skills to identify and bring faculty together around challenging issues which they then bring to their supervisors with a solutions-oriented approach. In some instances, after a few months in the role, some FWBCs were determined not to be the best fit and asked to step down in place of others.
The Associate Dean and CWO provide mentorship and training for the FWBCs to guide and coach them in their work to improve well-being in their departments. The program is also supported by both a program coordinator and research coordinator who assist with meeting planning, scheduling and resource distribution. Chairpersons are encouraged to provide incentives for the FWBC role but there is no mandatory compensation required. As a result, in the current state of the program, some FWBCs have salary support, some receive stipends or bonuses, some receive extra CME funds, while others remain financially unsupported for their role.
The FWBCs create a direct line of communication and collaboration to faculty across sites, departmental leaders, and our office. The roles of the FWBCs include (I) asking questions and listening to their departmental colleagues about the challenges and barriers to their well-being at work through individual discussion, focus groups or short surveys, (II) collating and summarizing data gathered into themes and priorities, (III) sharing the core themes and priorities with departmental leadership, and (IV) devising a plan and advocating for initiatives aimed at addressing those core priority areas. In our first iteration of the program, we created several resources for the FWBCs including a WBC manual that included: roles and responsibilities of the FWBC and curriculum goals and objectives, a focus group guide, and a top 10 list of effective interventions for well-being guide (Appendixes 1,2). FWBC are also asked to meet with their department chairperson at least twice per year (once with the CWO and Associate Dean present) and to meet with the Associate Dean and the other FWBCs once monthly.
In interactive 30-min monthly meetings led by the Associate Dean, FWBCs receive an interactive curriculum and the opportunity to share report-outs regarding the well-being challenges and programs in their departments. Approximately one half of the sessions each year incorporate the delivery of didactic or informational resource material while the other half is spent in discussion, including the sharing of best practices. The curricular elements focus on the evidence behind well-being and burnout in physicians, burnout intervention effectiveness, strategies to improve well-being and decrease burnout, and institutional resources that may help them in their work. The interactive monthly curriculum includes training in burnout and well-being assessments tools, effective systems- and personal-level well-being interventions, wellness-centered leadership skills, and information-sharing about institutional resources and programs with the potential to positively impact well-being. Report-outs include discussions of the current challenges to well-being in each department, outcomes from piloted interventions, and opportunities to brainstorm about department- and institution-level interventions.
We currently have approximately 37 faculty FWBC who represent 26 departments. Our eventual goal is to have all FWBCs compensated for their time and effort through their departments. Interestingly, there is a broad range of engagement of our FWBCs which does not necessarily correlate with the level of compensation they receive for their role. While attendance is not mandatory for the monthly meetings, monthly meetings are offered on two dates each month to maximize turnout. Certain departmental representatives have a harder time attending due to their schedules (such as certain surgical specialties); and because of this issue, we have created a surgical specialty group that meets quarterly at an earlier time to accommodate schedules. On average, 20–25 champions attend the meetings monthly.
GME WBC program
The Office of GME, in collaboration with the ISMMS GME Training Programs, created the GME WBC program in 2017. In this program, faculty members are appointed to work towards promoting a culture of well-being within a given residency or fellowship training program. The GME WBCs work in collaboration with the training program director, program administrator, and GME trainees (residents and fellows). GME WBCs are physician faculty members who specifically are not members of the GME training program leadership team. To ensure that well-being is prioritized among the many competing demands in academic medicine, the GME WBCs work to ensure that well-being efforts are incorporated into the daily operations of the training program in both curricular and extracurricular domains.
Our current GME WBC program consists of 50 faculty members representing 36 specialties across 8 hospital sites. The program is funded by the Office of GME and each GME WBC receives an annual stipend as compensation for their role. The GME WBC has several responsibilities, including identification of drivers that erode GME trainee well-being, establishing a residency/fellowship level well-being committee, development of a well-being curriculum, educating faculty and trainees about the importance of seeking mental health treatment when indicated, ensuring the availability of mental health resources, and serving as a role model for physician well-being to both faculty and trainees. For example, the GME WBC facilitates and/or leads well-being events and curricula, disseminates information about institutional well-being programs, and encourages participation in such programs. In addition, the GME WBC reviews program-specific data from the annual Accreditation Council for Graduate Medical Education (ACGME) resident/fellow survey and the ISMMS GME Well-being survey. By reviewing the data, the champion can gain a better understanding of areas for improvement within their program and develop systems- and program-level initiatives to enhance the well-being of our trainees.
The GME WBC program is overseen by both a Director of GME WBCs and the Associate Dean for GME Well-Being and Resilience. The Director and Associate Dean provide mentorship and training to the WBCs to facilitate their examining areas for change, including efforts to decrease the work intensity and clerical burden within a residency/fellowship program. Formal semi-annual and annual reports are submitted by the GME WBC to the Director and Associate Dean to document progress within each program. The WBCs are also evaluated regarding their performance on an annual basis by OWBR and GME leadership.
Further, the GME WBC is expected to serve as a member with active participation on the Program Evaluation Committee (PEC). The PEC plays a central role in the development of residency and fellowship training programs. The committee takes part in reviewing the program annually and guiding ongoing program improvement, including development of new goals, based on outcomes. As a member of the PEC, the GME WBC has an integral role within the residency or fellowship program.
Needs assessment
In order to create a robust and effective program to enhance the well-being of our faculty and trainees, we created a needs assessment survey for both constituencies. The following describes the survey methods for both faculty and trainees. For the purpose of this innovations report, we will present here brief descriptive data that drove our interventions.
Faculty survey
In 2018–2019, we developed and administered our first faculty well-being survey, which was conducted online as an anonymous, institution-wide effort, approved by our institutional IRB (18-01090). Participants reviewed a consent document at the beginning of the survey but did not have to sign consent as our IRB deemed the study exempt. The goal was to deliver this survey every other year; however, the second survey was put on hold due to coronavirus disease 2019 (COVID-19) and will be delivered again in 2022. Eligible participants in 2018–2019 included all 4,156 clinical and non-clinical faculty of the school, and survey items included demographics, burnout, resilience, and well-being indices, as well as potential current drivers of and solutions for burnout. The survey utilized the Maslach Burnout Inventory (MBI) 2-item scale (14), which assessed two dimensions of burnout (emotional exhaustion and depersonalization); the Mayo Well-Being Index, which assesses 7 dimensions of well-being (15); the CD-RISC 2-item scale (16), which assessed levels of resilience, elements of the mini-Z (17); the Mayo Leadership Index, which assessed leadership behaviors of respondents’ supervisors (18); as well as items on overall professional satisfaction, meaning in work and work-life balance (19). We also asked questions to evaluate quality of mentorship (20) and screened for depression using the PHQ-2 (21). In addition, we asked faculty to select from a list of potential systems- and personal-level interventions, informed in part by existing evidence, to indicate which they believed would most likely improve their well-being. Supplemental Appendix 3 details a list of questions and proprietary indices used in the 2018 faculty survey.
Residents and fellows survey
In 2018, 2019, and again in 2021, the GME Office developed and administered a GME well-being survey that was conducted throughout the healthcare system. The anonymous, online survey was approved by our institutional IRB (17-02885). Participants reviewed a consent document at the beginning of the survey but did not have to sign consent as our IRB deemed the study exempt. As with the faculty survey, the GME survey included the MBI 2-item scale, the PHQ-2, and questions surrounding meaning in work. The GME survey also included program-specific questions about systems-level well-being initiatives already in place. In 2017, the Accreditation Council for Graduate Medical Education (ACGME) revised its Common Program Requirements for all accredited residency and fellowship programs to include a section on well-being. The requirement stated that in partnership with the sponsoring institution, the program must include attention to scheduling, work intensity, work compression and efforts to minimize non-physician obligations that impact resident well-being. As a result, our Office of GME had already implemented a number of well-being initiatives. For example, residents and fellows were asked about utilization of wellness days, and if they knew how to access mental health resources for (I) themselves if they felt depressed or in need of emotional support or (II) their colleagues if found to be in emotional distress or experiencing suicidal ideation. Residents and fellows were also asked to select from a listing of individual-level and systems-level interventions, in part informed by existing evidence, which they believed would enhance their well-being. Data reported in this present manuscript are from the 2019 annual GME well-being survey. Appendix 4 details a list of questions and proprietary indices used in the 2019 trainee survey.
Analysis plan
For both surveys we present demographic and descriptive statistics of the items described above and in the supplemental chart. We also calculated indices including the Mayo Leadership Index, the PHQ-2 (positive if the answer to either question was yes), and the MBI-2 score (property of Mind Garden Inc for which we obtained the appropriate license). The Mayo Leadership Index was calculated using the approach in Dyrbye et al. (22) whereby scores on all 7 items were tallied for a total possible score of 45 and averaged across all participants. Higher scores indicate more effective well-being focused leadership behaviors.
Results
Faculty needs assessment
Of the 4,156 faculties invited to complete the inaugural survey, 1,870 responded (45% response rate). Demographic and descriptive data are shown in Table 1. A proportion of 27.4% of faculty met criteria for burnout on the MBI and 22% screened positive for depression on the PHQ-2. A proportion of 94.3% of faculty believe their work to be meaningful, yet only 65.9% of faculty reported satisfaction with their job. Of faculty working in a research setting, 13.9% reported “definitely” or “likely” to leave their position within the next two years; of these respondents, insufficient funding (23.2%) and pressures associated with their position (23.2%) were the top two reasons for leaving. Of faculty working in a patient care setting, 16.8% were “definitely” or “likely” to leave their position within the next two years; of these respondents, emphasis on metrics and performance over patient care (18.7%), frustration within the medical system (12.1%), and feeling that career interests were not being supported (11.8%) were the top three reasons for leaving.
Table 1
| Variables | N (%) or mean [SD] |
|---|---|
| Participant demographics | |
| Gender | |
| Female | 744 (47.6) |
| Male | 753 (48.2) |
| Non-binary/other gender minority | 4 (0.2) |
| Prefer not to say | 63 (4.0) |
| Missing | 306 |
| Age | |
| 20–39 years | 429 (27.6) |
| 40–59 years | 808 (52.0) |
| 60+ years | 317 (20.4) |
| Missing | 316 |
| Professional characteristics | |
| Faculty level | |
| Instructor | 91 (5.9) |
| Assistant professor | 748 (48.5) |
| Associate professor | 307 (19.9) |
| Professor | 260 (16.9) |
| Other | 135 (8.8) |
| Missing | 329 |
| Full-time status | |
| Full-time | 1,311 (83.4) |
| Part-time >60% | 128 (8.2) |
| Part-time <60% | 43 (2.7) |
| Voluntary | 89 (5.7) |
| Missing | 299 |
| Hours worked per week | |
| ≤40 | 268 (17.1) |
| 41–60 | 786 (50.0) |
| >60 | 517 (32.9) |
| Missing | 299 |
| Department† | |
| Anesthesiology, Perioperative & Pain Management | 102 (5.5) |
| Dermatology | 18 (1.0) |
| Emergency Medicine | 115 (6.1) |
| Family Medicine & Community Health | 29 (1.6) |
| Geriatrics & Palliative Medicine | 30 (1.6) |
| Medical Education | 19 (1.0) |
| Medicine | 339 (18.1) |
| Neurology | 50 (2.7) |
| Neurosurgery | 17 (0.9) |
| Obstetrics, Gynecology & Reproductive Services | 89 (4.8) |
| Ophthalmology | 24 (1.3) |
| Orthopedics | 25 (1.3) |
| Otolaryngology/Head & Neck Surgery | 14 (0.7) |
| Pathology | 48 (2.6) |
| Pediatrics | 108 (5.8) |
| Psychiatry | 157 (8.4) |
| Radiation Oncology | 13 (0.7) |
| Radiology | 57 (3.0) |
| Rehabilitation Medicine | 15 (0.8) |
| Surgery | 45 (2.4) |
| Urology | 18 (1.0) |
| Research Departments | 147 (7.9) |
| Depression, meaning, and resilience | |
| Depression (PHQ-2) | |
| Screen positive | 389 (22.0) |
| Screen negative | 1,382 (78.0) |
| Missing | 99 |
| Work I do is meaningful to me | |
| Disagree/strongly disagree | 41 (2.4) |
| Neither agree nor disagree | 58 (3.3) |
| Agree/strongly agree | 1,630 (94.3) |
| Missing | 141 |
| Resilience (CD-RISC-2) | 7.0 [1.3] |
| Missing | 147 |
| Burnout, work-life integration, and professional satisfaction | |
| Maslach Burnout Inventory | |
| Burned out | 470 (27.4) |
| Not burned out | 1,243 (72.6) |
| Missing | 157 |
| Mayo Well-Being Index | |
| Not well | 587 (34.2) |
| Well | 1,130 (65.8) |
| Missing | 153 |
| Work leaves enough time for family (WLI) | |
| Disagree/strongly disagree | 668 (38.7) |
| Neither agree nor disagree | 367 (21.3) |
| Agree/strongly agree | 691 (40.0) |
| Missing | 144 |
| Overall I am satisfied with my job (PS) | |
| Disagree/strongly disagree | 279 (16.2) |
| Neither agree nor disagree | 309 (17.9) |
| Agree/strongly agree | 1,138 (65.9) |
| Missing | 144 |
| What is the likelihood that you will leave your current research setting within the next 2 years? | |
| None | 136 (38.5) |
| Slight/moderate | 168 (47.6) |
| Likely/definite | 49 (13.9) |
| Missing | 1,517 |
| Primary reason you are considering leaving your current research setting within the next 2 years? | As |
| Insufficient funding | 50 (23.2) |
| Pressures associated with your position | 50 (23.2) |
| To spend more time with family | 16 (7.4) |
| Personal health problems | 2 (0.9) |
| A family member’s health problems | 2 (0.9) |
| To pursue administrative/leadership opportunities | 20 (9.2) |
| To pursue research or medical education opportunities | 9 (4.2) |
| I’m not considering leaving | 30 (13.9) |
| Other | 37 (17.1) |
| Missing | 1,654 |
| Likelihood that you will leave your current patient care setting within the next 2 years? | |
| None | 436 (31.0) |
| Slight/moderate | 733 (52.2) |
| Likely/definite | 236 (16.8) |
| Missing | 465 |
| Primary reason you are considering leaving your current patient care setting within the next 2 years? | |
| Frustration within the medical system | 117 (12.1) |
| Emphasis on metrics and performance over patient care | 181 (18.7) |
| Frustration with EHR | 30 (3.1) |
| Feeling overburdened with clerical work | 75 (7.8) |
| Frustration with insurance companies | 12 (1.2) |
| Do not enjoy caring for patients anymore | 11 (1.1) |
| Feeling that your career interests are not being supported | 114 (11.8) |
| Declining reimbursement for clinical care | 40 (4.1) |
| Personal health problems | 9 (0.9) |
| A family member’s health problems | 6 (0.6) |
| To pursue administrative/leadership opportunities | 76 (7.9) |
| To pursue research or medical education opportunities | 28 (2.9) |
| I’m not considering leaving | 120 (12.4) |
| Other | 147 (15.2) |
| Missing | 904 |
| What do you plan to do if you leave your current practice? | |
| Look for a different clinical/patient care opportunity and continue to work as a physician | 658 (69.7) |
| Look for a different job in medicine (e.g., admin, other) and no longer work as a physician | 110 (11.7) |
| Leave the practice of medicine altogether to pursue a different career | 38 (4.0) |
| Retire | 82 (8.7) |
| Other | 56 (5.9) |
| Leadership and mentorship | |
| Please indicate the title of your direct/immediate supervisor† | |
| Medical director of practice | 212 (12.8) |
| Division chief | 508 (30.6) |
| Department chair | 632 (38.0) |
| Institute director | 90 (5.4) |
| Other | 219 (13.2) |
| Leadership index score (overall) (see Figure 3 for breakdown of index) | 31.3 [10.2] |
| Missing | 236 |
| Do you have a mentor(s) for career development within the Mount Sinai Hospital System?† | |
| Yes | 437 (26.8) |
| No | 1,196 (73.2) |
| What are the barriers to obtaining a mentor?† | |
| No one with shared interests | 109 (5.83) |
| Lack of time on my part to find one | 259 (13.6) |
| Lack of time on the part of potential mentors | 130 (6.9) |
| Previous negative experiences with mentors | 32 (1.7) |
| No one to guide me in finding a mentor | 428 (22.9) |
| Not sure what I should look for in a mentor | 255 (13.6) |
| I do not want a mentor | 263 (14.1) |
| Other | 133 (7.1) |
| Overall, how satisfied are you with your mentor? | |
| Very dissatisfied/dissatisfied | 11 (2.5) |
| Neither satisfied nor dissatisfied | 29 (6.7) |
| Satisfied/very satisfied | 395 (90.8) |
| Missing | 1,435 |
†, numbers and percentages may not add up to 1,870 as some respondents did not answer all questions. PHQ-2, Patient Health Questionnaire-2; CD-RISC, Connor-Davidson Resilience Scale; WLI, work-life integration; PS, professional satisfaction; EHR, electronic health record.
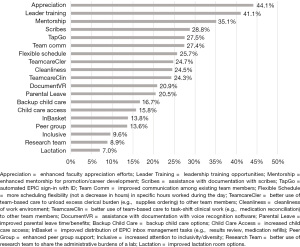
From a list of interventions that would most likely improve well-being, faculty identified improved appreciation (44.1%), enhanced mentorship (35.1%), documentation assistance (28.8%), enhanced teamwork (27.4% for improved communication among team members), and EHR solutions (27.5% for automatic EHR sign-in) as the top system-level interventions, while leadership training (41.1%) was the top individual-level intervention (Figure 2).
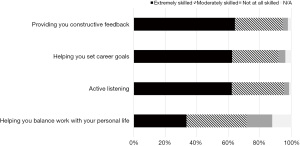
Overall, faculty rated their direct/immediate supervisor with a mean Mayo Leadership Index score of 31.4, a standard deviation of 10.2 and a range from 1 to 45. When examining the breakdown of leadership behaviors, leaders on average scored lowest on the following items: “holds career development conversation with me” (45% strongly agree/agree), “provides helpful feedback and coaching on my performance” (49% strongly agree/agree), and “encourages me to develop my talents and skills” (51% strongly agree/agree) (Figure 3). A proportion of 26.8% of faculty reported having a mentor for career development within the health system; 90.8% of these respondents were “very satisfied” or “satisfied with their mentor, with over 50% indicating that their mentor was “extremely skilled in” providing constructive feedback, setting career goals, and active listening (Figure 4). Of faculty without a mentor within the health system, no guidance in finding a mentor (22.9%), not wanting a mentor (14.1%), lack of time to find a mentor (13.6%), and not sure what to look for in a mentor (13.6%) were the top barriers listed.

Residents and fellows needs assessment
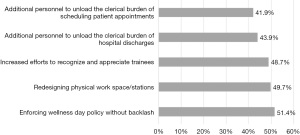
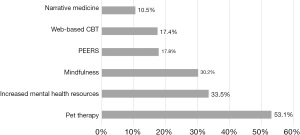
Of the 2,504 GME trainees asked to complete the 2019 survey, 1,415 responded (56.5% response rate). Demographic and descriptive data are shown in Table 2. Among the respondents, 54.8% met criteria for burnout on the MBI, down from 62.8% burnout on the prior 2018 survey. A positive PHQ-2 was identified in 33.1% of residents and fellows compared with 38.6% in the previous 2018 survey. A proportion of 69.9% of respondents indicated that their programs had a dedicated faculty member (i.e., WBC) who supports trainee well-being. Of a list of potential system-level interventions, GME trainees identified enforcing wellness day policies without backlash (51.4%), redesigning physical workspace/stations (49.7%), increasing efforts to recognize and appreciate trainees (48.7%), and reducing clerical burden (43.9% for hospital discharges, 41.9% for scheduling patient appointments) as what they believed most likely to improve their well-being (Figure 5). Pet therapy (53.1%) increased mental health resources (33.5%), and mindfulness (30.2%) were the top individual-level interventions identified as most likely to improve their well-being (Figure 6).
Table 2
| Variables | N (%) or mean [SD] |
|---|---|
| Participant demographics | |
| Gender† | |
| Female | 658 (47.3) |
| Male | 733 (52.7) |
| Non-binary/other gender minority | 2 (0.7) |
| Missing | 22 |
| Age | |
| ≤25 years | 12 (0.9) |
| 26–30 years | 786 (56.4) |
| 31–35 years | 490 (35.1) |
| ≥36 years | 106 (7.6) |
| Missing | 21 |
| Professional characteristics | |
| Average hours worked per week | |
| ≤70 | 920 (65.0) |
| 71–80 | 411 (29.0) |
| >80 | 84 (6.0) |
| Department† | |
| Anesthesiology | 120 (8.6) |
| Cardiovascular surgery | 10 (0.7) |
| Dermatology | 32 (2.3) |
| Dental & Oral Maxillofacial | 29 (2.1) |
| Emergency Medicine | 65 (4.7) |
| Family Medicine | 30 (2.2) |
| General Surgery and Subspecialties | 43 (3.1) |
| Internal Medicine and Subspecialties | 534 (38.3) |
| Neurology | 33 (2.4) |
| Neurosurgery | 18 (1.3) |
| Obstetrics & Gynecology | 49 (3.5) |
| Ophthalmology | 23 (1.6) |
| Orthopedic Surgery | 20 (1.4) |
| Otolaryngology | 22 (1.6) |
| Pathology | 31 (2.2) |
| Pediatrics | 63 (4.5) |
| Podiatry | 13 (0.9) |
| Physical Medicine & Rehabilitation | 13 (0.9) |
| Plastic Surgery | 12 (0.9) |
| Preventive Medicine | 9 (0.6) |
| Psychiatry | 142 (10.2) |
| Radiation Oncology | 9 (0.6) |
| Radiology | 58 (4.2) |
| Urology | 11 (0.8) |
| Vascular Surgery | 6 (0.4) |
| Depression, burnout, meaning, and Well-Being Champion program | |
| Depression (PHQ-2) | |
| Screen positive | 469 (33.1) |
| Screen negative | 946 (66.9) |
| Maslach Burnout Inventory | |
| Burned out | 775 (54.8) |
| Not burned out | 640 (45.2) |
| Work I do is meaningful to me† | |
| Disagree/strongly disagree | 86 (6.4) |
| Neither agree nor disagree | 60 (4.4) |
| Agree/strongly agree | 1,208 (89.2) |
| Does your program have a dedicated faculty member (i.e., Well-Being Champion) who supports trainee well-being? Yes | 989 (69.9) |
†, numbers and percentages may not add up to 1,415 as some respondents did not answer all. PHQ-2, Patient Health Questionnaire-2.
Intervention development
Using our survey results and literature on well-being interventions as a guide, our team, including the CWO, the Associate Deans for GME and Faculty Well-Being, the Dean of the School, and the Designated Institutional Official created an institutional plan to improve well-being for both the faculty and trainees. We (I) leveraged the WBC infrastructure as well as other institutional programs to guide the direction of future work and (II) created new programs and protocols to meet the well-being gaps of our faculty and trainees identified by the survey. While some well-being programming existed prior to survey development and dissemination, survey results informed enhancements to current programming as well as the development of new programs. Our process for creating the interventions included: (I) utilizing the survey data to determine core themes and priority areas, (II) devising potential strategies to improve these priority areas that were relatively low cost and required moderate effort with potential for moderate to high impact, (III) presenting potential solutions to leadership including the CWO, Dean of the School and the DIO, (IV) revising our intervention plan based on feedback and offered support from leadership, (V) piloting the interventions, and (VI) creating assessments and opportunities for feedback to then allow for iteration of the interventions.
Core themes and priorities
Three core areas for improving faculty well-being emerged from the survey: (I) documentation assistance and teamwork, (II) EHR and clerical work burden, and (III) leadership and mentorship initiatives that enhance career advancement and appreciation. These three identified core needs served as the basis for and were addressed by three interventions: (I) Faculty Well-Being Champion Departmental Plans, (II) EHR and Clerical Work Burden Reduction Programs and (III) Leadership and Mentorship Programming.
Three core areas for improving physician trainee well-being emerged from the GME survey: (I) increased, but not ubiquitous, presence of WBC in each program, (II) improved, but still high, burnout and depression rates, and (III) the importance of clear wellness day policies and access. These three identified core needs served as the basis for and were addressed by the following three interventions: (I) Expansion of the GME WBC Program, (II) Development of a Residency/Fellowship Well-Being Plan, and (III) Wellness Day Policy enforcement.
Faculty well-being interventions
WBC departmental plans
Upon review of our survey results, we streamlined our FWBC program and began to provide even more guidance on interventions focused on “efficiency of practice” (i.e., documentation assistance, teamwork, EHR and clerical work burden) and “culture of well-being” (i.e., leadership and mentorship initiatives that enhance career development and appreciation). This led to our development of a Departmental Well-Being Plan Template (Appendix 5) that is completed by all FWBCs.
The departmental well-being plan is now a core component of the FWBC Program. The plan aims to outline a department’s annual proposal to implement systems-level (efficiency of practice and cultural) well-being interventions. The process of creating a departmental well-being plan involves gathering data (i.e., system-wide faculty surveys, departmental-level surveys, focus groups, one-on-one discussions with faculty), choosing 2–3 priority areas based on data, and then brainstorming and choosing solutions based on the effort-impact matrix (23). We advise FWBCs and department chairs to consider solutions that serve multiple purposes, particularly in the domains of efficiency of practice, improvement of culture, and career advancement. We also advise FWBCs to lead a departmental well-being committee, which allows for representation across sites, divisions, and interests. Solutions are then devised using the collective efforts of the committee, WBC, department chair, and OWBR. Ideally, these departmental well-being plans are written and submitted to OWBR near the end of each calendar year, a time when departments create their budgets for the upcoming year. In this way, well-being interventions that may require financial support can be included in the annual budget. In addition, the CWO and Associate Dean can provide feedback and guidance regarding potential interventions, institutional resources, and evaluation planning.
Examples of some departmental-level solutions include the creation of more flexible schedules, mentorship programming (i.e., pairing junior faculty with senior faculty with similar interests), the hiring of scribes to reduce documentation burden, and devising team trainings and huddles to improve communication and clarify job roles. Additional efforts aimed at streamlining practice efficiency using the EHR are described in the next section.
EHR and clerical work burden reduction efforts
Our survey showed that faculty desire enhanced team-based care, better team communication, and more support for clerical burden to reduce burnout. In addition, our research demonstrated that more reported clerical burden (>60 min/day) and time on the EHR outside of work (>90 min/day) was associated with increasing levels of burnout (6). Since the advent of our office, the OWBR has partnered with information technology (IT) leadership and met regularly with IT to discuss challenges, goals, and potential IT/EHR solutions that could support faculty well-being. By establishing this collaboration, we were able to leverage our relationship to create interventions based on our needs assessment results. Two examples of programs born out of this collaboration were the EHR and Clerical Work Reduction Program and the InBasket Management Workgroup.
EHR and clerical work reduction grant program
In the peri-pandemic world, many ambulatory practices shifted to hybrid (in-person and telehealth) models of care. This transition required significant efforts from administrative and IT staff to redesign schedules and workflows, create novel EHR visit types, and manage insurance, billing, and compliance for virtual visits. The pandemic also greatly impacted the well-being of faculty and staff working on inpatient services and emergency departments as a result of staff shortages, workflow challenges, and ongoing clerical and documentation burdens. Prior research has demonstrated that increased clerical burden and ineffective teamwork is associated with decreased well-being and increasing levels of burnout (6,24).
To address these factors, the OWBR team devised the EHR and Clerical Work Reduction Grant program with the support of the Dean, to provide pilot grant funding to projects that aim to facilitate the reduction of EHR or clerical burden in ambulatory practices and promote efficiency in the work environments of clinical faculty. The expectation for the grant funding was to support pilot initiatives that demonstrated one of several potential impacts, including a shift of clerical or administrative burden away from clinical physicians, improved efficiency of the team, optimized EHR functionality, or enhanced team-based work and communication. The ultimate anticipated outcome of this grant program was to identify initiatives that (I) produce measurable effects on clinical faculty well-being and productivity, and (II) can be sustained and replicated across practices and departments.
In 2020, we began the grant application process. We created an application, assembled a review committee of 9 faculty experts in quality improvement, well-being, information technology and scholarship. We received 13 applications and after an initial and secondary review process, we awarded the inaugural grant funding to four projects that involved collaboration among faculty, departmental or divisional leaders, and clinical or administrative support staff in four departments and practice sites. Grant funding ranged from $25,000 to $80,000 for each project to be utilized over 18 months. The projects included (I) Creating and Disseminating a Principal Care Management Services Program of Billable, Coordinated Team Care for Patients With Chronic Conditions and Multiple Providers, (II) Enhancing Team-Based Care in Primary Care Geriatrics Practices through Patient Coordinators to Decrease Physician Burnout, (III) Optimizing InBasket management: An innovative team-based approach to digital patient care at Mount Sinai Doctors, and (IV) Promoting Telehealth Physician Wellness via Integrated Remote Team Workflow and Examination Technology. All projects are nearing the end of their grant funding and may publish their findings in the near future. A brief description of the Inbasket related projects is listed below.
InBasket Management Workgroup
The OWBR partnered with Mount Sinai Doctors Faculty Practice (physician practice group), IT, and our institutional and national EHR vendor representatives with the aim of reducing physician InBasket burden. This multidisciplinary team has worked on two main elements of the InBasket to reduce clerical burden: (I) InBasket structure and functionality, and (II) workflows for message triaging (particularly around patient calls and patient advice requests). Structural and functional changes have included updates to both patient- and provider-facing message views to improve communication and tracking of messages for care teams, as well as broadening the choices for patient subject lines (i.e., referral request, question about labs, appointment change, etc.) and updating messaging to patients to set clear expectations regarding types of questions patients can ask (nonurgent), when to expect a response (within two business days), and the team member who may respond to their message (physician or a staff member on the care team).
For message triaging, as part of the EHR grant program, two primary care practices were awarded funding to more efficiently route non-clinical InBasket messages away from the providers and towards trained staff members who can review and address requests in a timely fashion. The two practices were relatively small—3 to 8 providers. The smaller practice in which there existed a 1:1 provider to medical assistant ratio, utilized current staff to manage the Inbasket workflow. In this practice the grant funding was utilized to support 10% of the medical director’s and practice manager’s time to support their organizational and training work. The slightly larger practice hired 2 additional administrative members partially funded by the grant, to manage the message triaging. Staff were trained to address different messages and provide templated responses for typical requests. For example, messages regarding referral requests, medication refills, form requests, and appointment requests could all be handled by non-physician staff members. Workflows for this type of triaging included leveraging provider or practice levels staff pools or using the InBasket attach function. In addition, staff could also assist with clinical questions by scheduling patients into same or next-day urgent in-person or video visits, such that providers could fully assess new clinical questions during scheduled patient care time (as opposed to after-hours via messaging or phone calls).
The workgroup has also implemented a real-time InBasket management dashboard to help practices gain better insight into InBasket activity. The dashboard included the number of messages received by providers and staff in each InBasket folder, time to closure of the message, time spent in the InBasket, and other metrics. Data is currently being collected to assess reductions in the number of messages providers receive and time spent after hours working within the EHR InBasket folder.
Leadership and mentorship programming
Both mentorship and coaching can decrease burnout and stress, and higher rating of a leader’s feedback and coaching is correlated with lower burnout in their supervisees (18,25,26). Similarly, the effectiveness of a leader’s ability to show appreciation is inversely associated with burnout and can increase productivity and engagement of workers (18,27). In response to our faculty’s desire for greater mentorship and career development, and lower ratings of supervisors on their coaching and appreciation skills, faculty leadership workshops and increased mentorship programming were developed. A team of leadership and teaching experts from our Talent Development & Learning team (human resources department responsible for creating learning modules and programs for all employees), the Mount Sinai Doctors Faculty Practice, Office of Excellence in Patient Care (office led by the Chief Medical Officer to improve quality of patient care and patient experience) and the Associate Dean for Faculty Well-Being collaborated to create well-being focused leadership workshops. Over the course of a few months, the first two workshops which focused on the core leadership skills of coaching and appreciation were developed and piloted in February and March of 2020. Utilizing feedback from participants, these workshops were refined and subsequently delivered each fall and spring to over 300 faculty in total. Overall, these workshops were well-received by faculty leaders who participated and are currently being expanded in reach and scope to include additional sessions on the topics of Psychological Safety and Challenging Conversations (28). Further analysis is underway to assess the effectiveness and impact of these workshops on workplace culture and well-being.
In 2020, the OWBR partnered with the Office of Faculty Development (OFD) to further advance the quality and accessibility of mentorship for faculty across the institution. Currently, the OWBR-OFD teams are working on three core programs to enhance mentorship for faculty across the institution: (I) a web-based faculty mentor matching program, (II) the creation of a brief mentorship training curriculum for scientists and physicians, and the (III) enhancement of departmental mentoring leadership programs for which each department identifies one or more mentorship leaders responsible for overseeing departmental mentorship programs.
Residents and fellows
GME WBC program expansion
Given that the presence of a dedicated faculty member serving as a GME WBC may be associated with better outcomes for the well-being of residents, we have worked to expand the GME WBC program in the various residency and fellowships over the past 5 years to improve the trainee experience (29). While 69.9% of trainees in the 2019 survey identified their programs as having a dedicated WBC, we aspire to place a WBC in all training programs to meet trainee needs. The GME WBC focus areas have included: increasing protected time for educational activities, revising call schedules, and redesigning physical workspace and on-call rooms. The champions also direct efforts towards the restructuring of trainee clinics, EHR optimization, and decreasing documentation burden. Trainee professional development is another key focus area for the GME WBC. Programs conduct career and financial counseling sessions for graduating residents and fellows and integrate professional development style workshops on communications and team building into the GME trainee didactic curriculum.
Development of a Residency/Fellowship Well-Being Plan
The 2019 GME well-being survey results identified residency and fellowship programs within our healthcare system with high burnout (defined as burnout ≥70% of GME trainees) and high depression scores (defined as ≥40% of trainees). In an effort to have more focused discussions with leadership of these specific programs, leadership from OWBR and GME meet with the Program Director and GME WBC within these groups. The meetings create an opportunity for a collaborative discussion centered around well-being and are now part of an ongoing effort by the GME Office and OWBR to advance the well-being of trainees in all our programs.
As a mechanism to establish a more formal process to assist training programs, the GME Office and OWBR have created a template for residency and fellowship programs to develop plans to address trainee well-being with a continued focus on system-level initiatives. GME WBCs are asked to work in conjunction with residency/fellowship program leadership to design well-being infrastructure and a plan for their specific training programs. The development of a GME well-being plan is a stepwise process. An initial step is the formation of a residency/fellowship Well-Being Committee led by the GME WBC and consisting of trainee representatives. The GME WBC and program director then review relevant data (i.e., results from the ISMMS GME well-being survey, ACGME resident/fellow survey, training program survey, and focus groups with trainees) as part of the needs assessment.
Upon reviewing these data, 2–3 priority areas are identified to focus on system-level or program-level initiatives so that solutions can be implemented. Programs are encouraged to examine the efficiency of trainee workflow initiatives that lead to well-being. This can be effectuated in some instances even without additional resources by shifting existing resources or leveraging technology or novel workflows (e.g., rotation schedules, call schedules, EHR optimization, and creation of auto-populated patient visit templates). As part of the template for the residency/fellowship well-being plan, programs are also asked to detail how solutions will be implemented and assessed for success on an ongoing basis.
GME wellness days
The ACGME common program requirements have highlighted the importance of resident/fellow well-being. Each ACGME-accredited program is expected to provide appropriate tools for mental health self-screening and access to confidential, affordable mental health assessment, counseling, and treatment, including access to urgent and emergent care 24 h a day, 7 days a week (30).
In 2017, the ISMMS GME Office established the use of Wellness Days for our trainees. With this initiative, residents and fellows are given protected time to attend to their personal health and wellness, including medical, dental, and mental health appointments. Trainees are provided with four wellness days in addition to other leave time (including sick and vacation leave) each academic year. These wellness days are earned quarterly (one wellness day per quarter) and cannot be accrued or used to extend any other type of leave (vacation; sick or Family and Medical Leave Act; conference/educational). The wellness day process was structured with the goal of minimizing disruptions to both patient care and training, while allowing residents and fellows sufficient protected time for appropriate personal health maintenance and wellness. At our institution, wellness days can also be used to care for the child of a resident/fellow who has a health condition requiring treatment or supervision or to care for an ill family member (parent, spouse, or child) or partner, including medical, dental, and mental health appointments where the resident/fellow’s presence is needed.
Residency and fellowship programs are required to make every effort to accommodate a resident or fellow’s use of a wellness day during scheduled duties and are asked to establish policies and procedures that allow usage of this time. Programs are asked to track the wellness days utilization for each trainee; however, they do not require that residents and fellows provide documentation of appointments. Advance notice of at least seven days should be provided by the trainee to their Program Director or designee prior to using the wellness day so that adequate coverage can be ensured. Programs are encouraged to implement a system of coverage to ensure that use of wellness days does not produce an undue burden on other residents and faculty and minimizes disruptions to patient care and resident or fellow education. Since our health system has over 200 training programs that vary considerably in terms of size, scheduling systems, and coverage demands, individual programs are allowed flexibility in enabling the use of wellness days so long as policies and procedures are applied consistently.
Among the system-level interventions identified by GME trainees as likely to enhance their well-being, enforcing the wellness day policy without backlash was one of the highest interventions noted. In order to address this gap, the Office of GME and OWBR worked to change the culture by organizing public forums with key stakeholders (i.e., program directions, GME WBCs, and trainees). In these public settings, GME and OWBR leadership review the policy with all stakeholders and stress the importance of ensuring policy protection without backlash. The efficacy of this intervention is demonstrated by results from 2019 trainee well-being survey, in which 35.9% of trainees used 1–3 wellness days during the past 6 months of the survey (Figure 7), in comparison to 30.2% of trainees in 2018.
Discussion
The OWBR has seen the impact of burnout and psychological distress firsthand and has been at the forefront of initiatives around physician well-being, albeit with challenges related to the immense size and varied needs of our workforce. COVID-19 heightened the acuity of the well-being needs of physicians across the globe. Our own MSHS workforce, which for a time in the Spring of 2020 was at the epicenter of the global pandemic, has experienced elevated symptoms of depression, anxiety, post-traumatic stress disorder, and burnout across health professions (31,32). Now more than ever, we look to share well-being resources and lessons learned from our own experience with our regional, national, and international colleagues.
We summarize a three-pronged approach—creating infrastructure to promote well-being, distributing a needs assessment survey, and developing interventions in response to survey results—to address physician faculty and trainee well-being in a large urban healthcare system. Although well-being needs vary widely across settings, our institution found that faculty physicians most valued opportunities for leadership training, enhanced mentorship and career advancement, documentation assistance, and decreased electronic health record and clerical burden, while trainee physicians most valued enforcement of the wellness day policy without backlash. Both groups valued improved appreciation efforts. These survey results have informed numerous interventions to improve the well-being of both our faculty and trainees. For our faculty, these interventions have included (I) annual faculty well-being departmental plans, (II) implementation of EHR clerical work burden reduction programs, and (III) enhancement of our leadership and mentorship programming via new and enhanced training programs. For our trainees, these interventions have included (I) expansion of our GME well-being champions program, (II) development of trainee well-being plans, and (III) implementation of protected wellness days for all trainees.
Beyond MSHS, other peer institutions are doing similar work, such as Vanderbilt University Medical Center (VUMC) and Weill Cornell Medicine. VUMC assembled a taskforce that developed a five-step approach to implement recommendations supporting and measuring physician well-being, and they closely monitored the progress via validated survey metrics (33). Similarly, using surveys and focus groups, Weill Cornell developed a Top 10 list of tenets to inform their grassroots approach to building a more nurturing, supportive environment for physicians and their clinical care teams, and they have measured their progress over time using the Mayo Clinic Well-Being Index (7).
Our current work is limited in that we have not yet evaluated the impact of all our interventions, and there are likely multiple confounding factors in assessing their effects. In addition, our survey findings are specific to a single institution in one geographic region; however, we identify a three-pronged approach that can be generalized and implemented across many types of institutions.
Conclusions
This article summarizes the well-being needs assessment and systems-level interventions for faculty and GME trainee physicians at a large urban healthcare system in New York City. The OWBR and other collaborators have supported enhancements to existing well-being infrastructure, which addressed the needs of our constituents as captured in the surveys and established the foundational structure to support the longevity of these interventions. Although this work is challenging, our data supports the increasing importance of prioritizing the well-being of healthcare providers. Future work will continue to focus on the collection of well-being, burnout, and other professional fulfillment data to assess the impact of our interventions and to enhance our understanding of the needs of our physician community. Our hope is that other institutions recognize the value of this work and consider implementing similar data-informed interventions to enhance physicians’ and medical trainees’ sense of well-being and professional fulfillment—enabling them to deliver high quality, effective, and compassionate patient care while feeling cared for in their workplace.
Acknowledgments
The authors wish to thank Dr. Dennis Charney; Dr. Michael Leitman; the Graduate Medical Education (GME) Office at the Icahn School of Medicine at Mount Sinai (ISMMS); ISMMS GME and Faculty Well-being Champions; ISMMS EHR and Clerical Burden Reduction Grant Steering Committee and Grantees; ISMMS Residents, Fellows, and Faculty; Mount Sinai Health System (MSHS) Talent Development and Learning; Mount Sinai Doctors Downtown; Mount Sinai Doctors Faculty Practice and Commitment to Caring Program; Mount Sinai Office of Excellence in Patient Care; MSHS and ISMMS Information Technology Teams; Office of Faculty Development at ISMMS; Office of Well-Being and Resilience at ISMMS; and all of the participants at the Mount Sinai Hospital who completed the survey.
Funding: This study was supported by internal funding from the Icahn School of Medicine at Mount Sinai.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Stephen J. O’Connor, Nancy Borkowski and Katherine A. Meese) for the series “Shaping Tomorrow’s Healthcare Systems: Key Stakeholders’ Expectations and Experiences” published in Journal of Hospital Management and Health Policy. The article has undergo external peer review.
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-47/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-47/coif). The series “Shaping Tomorrow’s Healthcare Systems: Key Stakeholders’ Expectations and Experiences” was commissioned by the editorial office without any funding or sponsorship. LP received honoraria for speaking engagements at Atrium Health Wake Forest Baptist, American Society of Health-System Pharmacists, Stanford University, and the University of Montana. JR received honoraria for numerous speaking engagements at professional societies, academic medical centers, healthcare institutions; worked as a consultant for the well-being program at the NYU School of Medicine Long Island; served as a non-fiduciary board member of the Lorna Breen Foundation; and served on a temporary advisory board established by PEPSICO to inform employee well-being efforts. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of the Icahn School of Medicine at Mount Sinai (No. 18-01090 for faculty survey, 17-02885 for graduate medical education survey) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Murthy V. Addressing Health Worker Burnout – The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. Current Priorities of the U.S. Surgeon General 2022. Available online: https://www.hhs.gov/surgeongeneral/priorities/health-worker-burnout/index.html
- Shanafelt TD, West CP, Sinsky C, et al. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2020. Mayo Clin Proc 2022;97:491-506. [Crossref] [PubMed]
- Rodrigues H, Cobucci R, Oliveira A, et al. Burnout syndrome among medical residents: A systematic review and meta-analysis. PLoS One 2018;13:e0206840. [Crossref] [PubMed]
- Lacy BE, Chan JL. Physician Burnout: The Hidden Health Care Crisis. Clin Gastroenterol Hepatol 2018;16:311-7. [Crossref] [PubMed]
- Zhang X, Wang J, Hao Y, et al. Prevalence and Factors Associated With Burnout of Frontline Healthcare Workers in Fighting Against the COVID-19 Pandemic: Evidence From China. Front Psychol 2021;12:680614. [Crossref] [PubMed]
- Peccoralo LA, Kaplan CA, Pietrzak RH, et al. The impact of time spent on the electronic health record after work and of clerical work on burnout among clinical faculty. J Am Med Inform Assoc 2021;28:938-47. [Crossref] [PubMed]
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med 2018;283:516-29. [Crossref] [PubMed]
- Kjaer K, Kowalsky R, Rubin LA, et al. A Grassroots Approach to Protecting Physicians Against Burnout and Building an Engaging Practice Environment. NEJM Catalyst Innovations in Care Delivery 2021;2: [Crossref]
- West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388:2272-81. [Crossref] [PubMed]
- Panagioti M, Panagopoulou E, Bower P, et al. Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis. JAMA Intern Med 2017;177:195-205. [Crossref] [PubMed]
- National Academies of Sciences, Engineering, and Medicine, National Academy of Medicine, Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. Taking Action against Clinician Burnout: A Systems Approach to Professional Well-Being. National Academies Press; 2019.
- Thomas Craig KJ, Willis VC, Gruen D, et al. The burden of the digital environment: a systematic review on organization-directed workplace interventions to mitigate physician burnout. J Am Med Inform Assoc 2021;28:985-97. [Crossref] [PubMed]
- Brower KJ, Brazeau CMLR, Kiely SC, et al. The Evolving Role of the Chief Wellness Officer in the Management of Crises by Health Care Systems: Lessons from the Covid-19 Pandemic. NEJM Catal Innov Care Deliv 2021;2: [Crossref]
- Li-Sauerwine S, Rebillot K, Melamed M, et al. A 2-Question Summative Score Correlates with the Maslach Burnout Inventory. West J Emerg Med 2020;21:610-7. [Crossref] [PubMed]
- Dyrbye LN, Varkey P, Boone SL, et al. Physician satisfaction and burnout at different career stages. Mayo Clin Proc 2013;88:1358-67. [Crossref] [PubMed]
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003;18:76-82. [Crossref] [PubMed]
- Olson K, Sinsky C, Rinne ST, et al. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress Health 2019;35:157-75. [Crossref] [PubMed]
- Shanafelt TD, Gorringe G, Menaker R, et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc 2015;90:432-40. [Crossref] [PubMed]
- Sinsky CA, Dyrbye LN, West CP, et al. Professional Satisfaction and the Career Plans of US Physicians. Mayo Clin Proc 2017;92:1625-35. [Crossref] [PubMed]
- Fleming M, House S, Hanson VS, et al. The Mentoring Competency Assessment: validation of a new instrument to evaluate skills of research mentors. Acad Med 2013;88:1002-8. [Crossref] [PubMed]
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003;41:1284-92. [Crossref] [PubMed]
- Dyrbye LN, Major-Elechi B, Hays JT, et al. Relationship Between Organizational Leadership and Health Care Employee Burnout and Satisfaction. Mayo Clin Proc 2020;95:698-708. [Crossref] [PubMed]
- Mind Tools Content Team. The Action Priority Matrix: Making the most of your opportunities. Time Management Tools From MindTools.com. Available online: https://www.mindtools.com/pages/article/newHTE_95.htm
- Whitmore J. Coaching for performance. 5th ed. London: Nicholas Brealey; 2017.
- Zhang H, Isaac A, Wright ED, et al. Formal mentorship in a surgical residency training program: a prospective interventional study. J Otolaryngol Head Neck Surg 2017;46:13. [Crossref] [PubMed]
- Dyrbye LN, Shanafelt TD, Gill PR, et al. Effect of a Professional Coaching Intervention on the Well-being and Distress of Physicians: A Pilot Randomized Clinical Trial. JAMA Intern Med 2019;179:1406-14. [Crossref] [PubMed]
- Grant AM, Gino F. A little thanks goes a long way: Explaining why gratitude expressions motivate prosocial behavior. J Pers Soc Psychol 2010;98:946-55. [Crossref] [PubMed]
- Peccoralo L, Johnson C, Kaplan C, et al. A Coaching and Appreciation Workshop for Faculty Leaders to Enhance Faculty Well-being and Engagement. Poster Presentation, American Conference on Physician Health, Scottsdale, AZ, October 8, 2021
- Bui AH, Ripp JA, Oh KY, et al. The impact of program-driven wellness initiatives on burnout and depression among surgical trainees. Am J Surg 2020;219:316-21. [Crossref] [PubMed]
- Accreditation Council for Graduate Medical Education. Common Program Requirements, 2022. Available online: https://www.acgme.org/what-we-do/accreditation/common-program-requirements/
- Feingold JH, Peccoralo L, Chan CC, et al. Psychological Impact of the COVID-19 Pandemic on Frontline Health Care Workers During the Pandemic Surge in New York City. Chronic Stress 2019;5:2470547020977891. [Crossref] [PubMed]
- Peccoralo LA, Pietrzak RH, Feingold JH, et al. A prospective cohort study of the psychological consequences of the COVID-19 pandemic on frontline healthcare workers in New York City. Int Arch Occup Environ Health 2022;95:1279-91. [Crossref] [PubMed]
- Yakes EA, Dean S, Labadie RF, et al. Factors Associated With Physician Empowerment and Well-being at an Academic Medical Center. J Occup Environ Med 2020;62:478-83. [Crossref] [PubMed]
Cite this article as: Peccoralo L, Tong M, Kaplan S, Ripp J, Akhtar S. Strategies for enriching the resident, fellow, and faculty physician experience: a system-based approach to physician well-being. J Hosp Manag Health Policy 2022;6:35.