Analysis of dual degree, gender, and specialty on obtaining leadership positions in academic settings: a multi-institutional study
Introduction
To address the leadership challenges of the modern healthcare landscape, many United States medical schools have offered a variety of dual degree programs (1). Pursuing a specific degree may be driven by a desire to gain the skills to perform research at the highest level, improve leadership skills, or enhance policy-making abilities. Additionally, these degrees could serve as tools to augment a physician’s sphere of influence in the academic setting.
Currently, little is known about whether dual degrees are more prominent amongst physicians in leadership roles. This study sought to evaluate the present state of medical leadership by investigating the prevalence of advanced degrees in medical leadership, while also examining the gender equality and specialty distribution among those in leadership. We present the following article in accordance with the STROBE reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-91/rc).
Methods
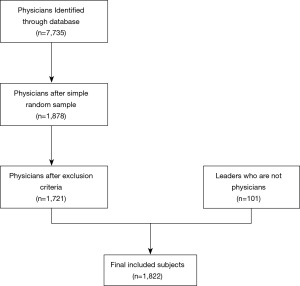
In this cross-sectional study, the physicians from six University of California (UC) hospitals and medical schools were compiled from the UC database for employee pay (https://ucannualwage.ucop.edu/wage) for the most recently released year at the time of research (2018): UC Davis, UC San Francisco, UC Riverside, UC Los Angeles, UC Irvine, and UC San Diego. After 7,735 subjects were identified, simple random sampling of 360 subjects from each of the 6 universities and exclusion of non-physicians or non-practicing physicians resulted in 1,721 physicians included for final study (Figure 1). Physicians were designated most commonly by the titles of “PROF OF CLIN-HCOMP” (Professor of Clinical-Health Sciences Compensation Plan) or “PROF-HCOMP,” (Professorial-Tenure-Health Sciences Compensation Plan) in the UC database for employee pay, with any unclear cases being confirmed through searches on official university websites.
Simultaneously, 315 medical leadership roles were identified through reviews of institutional websites and publicly available organization charts. These roles were classified into three categories: hospital leadership, medical education leadership, and department leadership. Hospital leadership included roles such as Chief Executive Officer, Chief Financial Officer, Chief Medical Officer. Medical Education Leadership included positions such as Dean, Vice Dean, Associate Dean, and Assistant Dean positions. Department Leadership included positions such as Chair of the Department. All leaders, regardless of whether or not they were medical physicians, were included in this study. Advanced degrees were defined as any degree, in addition to an MD, that required schooling beyond an undergraduate degree (i.e., master’s or doctoral degree). The specific degrees were recorded, as well as those who possessed multiple advanced degrees. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional review board approval and informed consent were not required as the present study conducted a retrospective review of publicly available data.
Statistical analysis
Descriptive statistics and Pearson’s chi-square test were used with a 5% level of significance to determine the influence of degree, gender, or specialty in medical leadership.
Results
Of 315 identified medical leadership roles, 214 (67.9%) were held by physicians. Among physicians in leadership roles, 74 (34.6%) had dual degrees compared to 436 (25.3%) without leadership roles (P<0.001) (Figure 2A). The most popular advanced degrees amongst physician in leadership roles included the PhD (34, 24.8%), MPH (16, 11.7%), and MBA (8, 5.8%) (Table 1). Although 30 physicians (1.74%) in this dataset possessed a DO degree, no DO physicians held leadership roles.
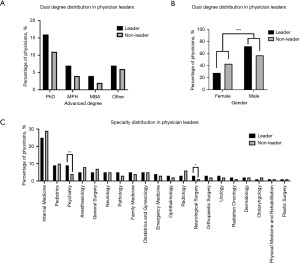
Table 1
| Variable | Comparison | P value |
|---|---|---|
| Dual degree | ||
| MD/Anya | MD only | <0.001*** |
| MD/PhD | MD only | 0.019* |
| MD/MPH | MD only | 0.009** |
| MD/MBA | MD only | 0.042* |
| MD/Otherb | MD only | 0.157 |
| MD/PhD | MD/MBA | 0.462 |
| MD/PhD | MD/MPH | 0.443 |
| MD/MBA | MD/MPH | 0.894 |
| Gender | ||
| Female | Male | <0.001*** |
| Specialty | ||
| Internal Medicine | All other specialties | 0.197 |
| Pediatrics | All other specialties | 0.668 |
| Psychiatry | All other specialties | 0.003** |
| Anesthesiology | All other specialties | 0.191 |
| General Surgery | All other specialties | 0.433 |
| Neurology | All other specialties | 0.882 |
| Pathology | All other specialties | 0.179 |
| Family Medicine | All other specialties | 0.832 |
| Obstetrics and Gynecology | All other specialties | 0.900 |
| Emergency Medicine | All other specialties | 0.213 |
| Ophthalmology | All other specialties | 0.465 |
| Radiology | All other specialties | 0.158 |
| Neurological Surgery | All other specialties | 0.019* |
| Orthopaedic Surgery | All other specialties | 0.391 |
| Urology | All other specialties | 0.391 |
| Radiation Oncology | All other specialties | 0.184 |
| Dermatology | All other specialties | 0.686 |
| Otolaryngology | All other specialties | 0.826 |
| Physical Medicine and Rehabilitation | All other specialties | 0.879 |
| Plastic Surgery | All other specialties | 0.797 |
*, P<0.05; **, P<0.01; ***, P<0.001. a, any advanced degree; b, other advanced degrees besides PhD, MPH, or MBA.
Females held significantly fewer leadership roles than males (28.0% vs. 72.0%; P<0.001). While the baseline of physicians not in leadership also contained less females than males overall (42.8% vs. 57.2%; P<0.001), females were still significantly underrepresented in leadership when compared to this baseline proportion of females not in leadership (28.0% vs. 42.8%; P<0.001) (Figure 2B). When comparing those with and without advanced degrees, there was no difference in the representation of females (40.1% vs. 41.2%; P=0.684).
The three most common specialties overall included Internal Medicine (497, 28.9%), Pediatrics (172, 10.0%), and Anesthesia (119, 7.7%) (Figure 2C). The three most common specialties amongst physician in leadership roles were Internal Medicine (53, 24.6%), Pediatrics and Psychiatry (both with 19, 9.0%). Neurosurgery (2.8% vs. 1.0%; P=0.019) and Psychiatry (9.0% vs. 4.4%; P=0.003) had a significantly higher percentage of physicians in leadership roles compared to physicians not in leadership roles within their specialty.
Discussion
This study found significant associations between physicians in leadership roles and having a PhD, MBA, and MPH, though there was no statistical significance between these degrees. Despite equal gender representation amongst physicians with advanced degrees, females were significantly underrepresented in leadership. Internal Medicine physicians held the highest percentage of leadership roles, but this could be attributed to a larger number of internists within these data. Two-thirds of medical leadership roles were held by physicians, reinforcing conclusions from previous studies that having a clinical background is a crucial component of becoming an effective medical leader (2-4).
As early as medical school, physicians and physicians-in-training are exposed to the organizational burdens of healthcare. Regardless of specialty, doctors play a leading role in the healthcare team and are often the final responsible entity for the overall outcome of patient care (5-7). Navigating this responsibility requires a comprehensive understanding of the political, economic, social, and technological drivers of healthcare, an understanding that often comes from pursuing an additional degree. Obtaining an MBA degree has often been cited as a competitive advantage for physicians in leadership positions (both for obtaining and succeeding in particular roles) (8,9), but our study also reveals the potential utility of the PhD and MPH for similar purposes (10,11).
Looking towards the future, medical education pathways have already begun to integrate leadership and management training into their curricula, with models being adapted for attending physicians as well (5,12,13). Programs that have been most successful have integrated leadership training not only longitudinally, but also by using areas of training that overlap with existing curricular content (9,14). Available evidence has suggested that physicians who do pursue a PhD, MBA, or MPH experience a greater level of professional advancement whether measured by leadership positions, publications, grant funding, or reimbursement (15). As healthcare continues to evolve in the 21st century, well-designed and well-evaluated leadership curricula are necessary.
To achieve this, it is important to understand the varied motivations behind pursuing different advanced degrees. Business-oriented skills provided by MBA training, such as finance and organizational management, are major considerations for medical trainees to pursue an MD/MBA (8). Moreover, as an MBA is recognized as one of the most suitable management degrees by and for physicians (16), those who recognize deficiencies in their management skills while navigating the complexity of modern healthcare may opt to receive MBA training during their post-residency career. With regards to an MPH, pre-medical students with an interest in public health and disease and medical students with intentions to enter academic practice were more likely to complete an MD/MPH (17). Physicians who chose to pursue an MPH after medical school commonly identified research training as one of the most powerful attractions towards public health curricula (18). Similarly, surveys of MD/PhD students at the University of Pennsylvania suggested that most students intend to enter academic medicine with a focus on research (19), and a survey study in Canada identified that physicians who received PhD training after medical school had a stronger focus on research compared to physicians who completed MD/PhD program or PhD before medical school matriculation (20). Together, literature provides preliminary evidence into when and why certain dual degrees are pursued by healthcare professionals, but further research is needed to effectively integrate advanced degree interests and leadership training to cultivate future generations of physician executives.
Along with our dual-degree investigations, we identified a clear gender disparity among physician leaders. Although the baseline representation of dual-degree individuals was similar among males and female physicians, females were underrepresented in leadership overall. This result is in line with previous studies demonstrating underrepresentation of women in leadership (21,22). Despite the significant association between possessing dual degrees and leadership positions overall, the added benefit of additional training among female physicians does not seem to confer the same advantages as it does for their male counterparts. Further study is needed to delineate potentially systemic barriers preventing equally qualified women from obtaining leadership roles.
There is a paucity of literature describing the distribution of medical specialty in physician leadership. We herein report the specialty characteristics of physician leadership in academic medical institutions within the University of California Health, with the observation that psychiatrists and neurosurgeons were overrepresented in clinical leadership. In a 2016 article, Goodall concluded that psychiatric leaders may enhance organizational performance in part through setting proper goals and establishing a supportive environment (23), and a study conducted by Fares et al. reported that the strict medical standards and management skills occupied by academic neurosurgeons makes them strong leadership candidates (24). Despite the literature support for our findings, more studies analzying other academic institutions and different institution types are needed to assess whether psychiatry and neurological surgery are associated with stronger leadership representation and a better understanding of the mechanism is needed. By identifying these qualities that may bestow a greater prediction for and competency in leadership positions, targeted training programs to future physician administrators can be applied across any specialty.
Overall, as this study can only identify characteristics of those in leadership based on the publicly available data, further study is required to determine causation, i.e., whether these characteristics provide an advantage for obtaining a leadership role. Additionally, further study is required to determine whether bias or local or system-wide barriers had an impact on the differences seen amongst characteristics such as gender (25).
Conclusions
Disparities in advanced degrees, gender, and specialty for medical leadership in academia have not been previously described. Our study explored the current disparities in healthcare management by analyzing whether various advanced degrees, specialties, or gender were associated with physicians in leadership in order to achieve equal representation and diversity. The MBA, MPH, and PhD degrees, along with Neurosurgery and Psychiatry specialties, were strongly associated with physicians in leadership, while females were largely underrepresented in leadership. These insights may be applied to address gaps in equity in other healthcare leadership settings to build more diverse administrative teams.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-91/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-91/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-91/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-91/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional review board approval and informed consent were not required as the present study conducted a retrospective review of publicly available data.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Crites GE, Ebert JR, Schuster RJ. Beyond the dual degree: development of a five-year program in leadership for medical undergraduates. Acad Med 2008;83:52-8. [Crossref] [PubMed]
- Llewellyn S. “Two-way windows”: Clinicians as medical managers. Organ Stud 2001;22:593-623.
- Berghout MA, Fabbricotti IN, Buljac-Samardžić M, et al. Medical leaders or masters?-A systematic review of medical leadership in hospital settings. PLoS One 2017;12:e0184522. [Crossref] [PubMed]
- Dine CJ, Kahn JM, Abella BS, et al. Key elements of clinical physician leadership at an academic medical center. J Grad Med Educ 2011;3:31-6. [Crossref] [PubMed]
- Chen TY. Medical leadership: An important and required competency for medical students. Ci Ji Yi Xue Za Zhi 2018;30:66-70. [Crossref] [PubMed]
- Satiani B, Sena J, Ruberg R, et al. Talent management and physician leadership training is essential for preparing tomorrow's physician leaders. J Vasc Surg 2014;59:542-6. [Crossref] [PubMed]
- Schwartz RW, Pogge C. Physician leadership: essential skills in a changing environment. Am J Surg 2000;180:187-92. [Crossref] [PubMed]
- Turner AD, Stawicki SP, Guo WA. Competitive Advantage of MBA for Physician Executives: A Systematic Literature Review. World J Surg 2018;42:1655-65. [Crossref] [PubMed]
- Ackerly DC, Sangvai DG, Udayakumar K, et al. Training the next generation of physician-executives: an innovative residency pathway in management and leadership. Acad Med 2011;86:575-9. [Crossref] [PubMed]
- Reilly JM, Plepys CM, Cousineau MR. Dual MD-MPH Degree Students in the United States: Moving the Medical Workforce Toward Population Health. Public Health Rep 2021;136:640-7. [Crossref] [PubMed]
- Andriole DA, Whelan AJ, Jeffe DB. Characteristics and career intentions of the emerging MD/PhD workforce. JAMA 2008;300:1165-73. [Crossref] [PubMed]
- Lazarus A. Why an MBA? Physician Exec 1997;23:41-5.
- Hopkins J, Fassiotto M, Ku MC, et al. Designing a physician leadership development program based on effective models of physician education. Health Care Manage Rev 2018;43:293-302. [Crossref] [PubMed]
- Hollis RJ, Pockros BM, Chen L. The MBA in Medical Education: Current MD/MBA Student Aspirations, Perceptions, and Motivations. J Surg Res 2021;259:305-12. [Crossref] [PubMed]
- Hall JF. Advanced degrees in academic colorectal surgery. Clin Colon Rectal Surg 2013;26:250-3. [Crossref] [PubMed]
- Hilsenrath PE. Healthcare management education settings in the United States: History and perspective J Manag Hist 2012;18:386-401.
- Andriole DA, Jeffe DB, Tai RH. Characteristics and Career Intentions of MD-MPH Program Graduates: A National Cohort Study. Public Health Rep 2016;131:637-49. [Crossref] [PubMed]
- Zweigenthal VE, Marquez E, London L. 'Why do an MPH?' Motivations and intentions of physicians undertaking postgraduate public health training at the University of Cape Town. Glob Health Action 2016;9:32735. [Crossref] [PubMed]
- Watt CD, Greeley SA, Shea JA, et al. Educational views and attitudes, and career goals of MD-PhD students at the University of Pennsylvania School of Medicine. Acad Med 2005;80:193-8. [Crossref] [PubMed]
- Kearney RA, Lee SY, Skakun EN, et al. The research productivity of Canadian physicians: how the timing of obtaining a PhD has an influence. Acad Med 2007;82:310-5. [Crossref] [PubMed]
- Skinner H, Burke JR, Young AL, et al. Gender representation in leadership roles in UK surgical societies. Int J Surg 2019;67:32-6. [Crossref] [PubMed]
- Moghimi S, Khurshid K, Jalal S, et al. Gender Differences in Leadership Positions Among Academic Nuclear Medicine Specialists in Canada and the United States. AJR Am J Roentgenol 2019;212:146-50. [Crossref] [PubMed]
- Goodall AH. A theory of expert leadership (TEL) in psychiatry. Australas Psychiatry 2016;24:231-4. [Crossref] [PubMed]
- Fares Y, Fares J, Kurdi MM, et al. Physician leadership and hospital ranking: Expanding the role of neurosurgeons. Surg Neurol Int 2018;9:199. [Crossref] [PubMed]
- Mangurian C, Linos E, Sarkar U, et al. What’s holding women in medicine back from leadership. Harvard Business Review, June 19, 2018, Updated November 07, 2018.
Cite this article as: Azzam DB, Sharma AN, Meller LLT, Noarbe B, Chin K, Torres J, Sharma SN, Wiechmann W. Analysis of dual degree, gender, and specialty on obtaining leadership positions in academic settings: a multi-institutional study. J Hosp Manag Health Policy 2022;6:37.