
Pairing a medical scribe with a hospitalist physician improved clinician satisfaction, increased productivity and provided a return on investment
Introduction
Medical scribes have been widely employed as personal productivity assistants in emergency departments (EDs) and ambulatory care clinics for years (1,2). In these settings, it has been demonstrated that medical scribes can increase clinician satisfaction and improve productivity (3,4). Similar findings have not been well-established in the hospitalist setting (5,6). While addition of a scribe to a hospitalist team utilizing industry data has been suggested as beneficial, we found no data showing actual measurement of outcomes with such an implementation (7). Could scribes increase hospitalist productivity while remaining financially feasible? If so, are the other benefits of scribe utilization described in the literature applicable to scribe utilization in a hospitalist admission shift?
Clinician satisfaction incorporates the growing challenge of physician burnout. Physician burnout has been well described by Maslach as a combination of depersonalization, lower personal accomplishment and emotional exhaustion (8). Burnout has likewise been associated with increased medical errors, decreased work effort, lower patient satisfaction and longer post discharge recovery times (9-11). Scribes have previously been shown to improve all aspects of physician satisfaction in the outpatient clinic (12). Hospital medicine literature indicates a burnout symptom rate prevalence of approximately 30% across all clinicians (13,14). Would addition of a scribe to a hospitalist admission service decrease clinician burnout?
Despite the known benefit to other services, there is a paucity of studies in the literature examining scribe deployment as an approach to reducing burnout in hospital medicine (15). We also found no research supporting that fact that burnout rates differ between hospitalist shift types (14). While the literature is lacking, anecdotal evidence suggests that hospitalist clinicians tend to avoid certain shift types, including swing and night shifts, and that this further increases burnout risk. To assess these problems with both workload and provider satisfaction, we attempted to employ a scribe on a hospitalist admission shift for an 8-week pilot. Our goal was to measure both productivity and provider satisfaction to determine both tangible and intangible benefits. We present the following article in accordance with the MDAR reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-26/rc).
Methods
We selected a bustling 280-bed community hospital for our pilot. With ED volumes averaging 80,000 visits per year, and daily admissions to the hospitalist team averaging 45 patients, there was notable opportunity for improvement in ED to inpatient throughput. We identified that a demand-capacity mismatch existed for the 12-hour physician swing shift. This shift was known to be highly stressful and had been historically avoided by many hospitalist team members. We hypothesized that pairing a medical scribe with a physician during this swing shift could have significant benefit. To test this hypothesis, we paired a medical scribe with the hospitalist physician who was performing serial admissions during the 12-hour swing shift. Data was collected over a 6-week period of time. The impact of the intervention on clinician satisfaction and productivity was quantified and return on investment (ROI) was calculated.
The use of a hospitalist medical scribe was hypothesized to be a means of addressing demand-capacity mismatch for swing shift clinicians who were facing high admission volumes. The swing shift was staffed with one physician from 11 a.m. to 11 p.m. During this time, the physician was performing serial admissions, and had no inpatient rounding duties. The physician was responsible for performing the admission and providing subsequent care until the end of the shift. The physician was assisted by an advanced practice clinician who was also performing serial admissions with an overlapping shift from 6 a.m. to 6 p.m. Despite the assistance of the advanced practice clinician, the swing shift physician was frequently working an additional 2 hours to continue admitting patients and to finalize electronic medical record documentation. This unmet demand resulted in heavy front-end admission burden for the oncoming nocturnist, congestion in the ED and diminished clinician satisfaction.
The use of a hospitalist medical scribe during a swing shift was also recognized as a potential means of reducing unbillable encounters. The number of patients who presented before midnight, but who were not seen by a clinician until after midnight, was high, resulting in a significant number of non-billable encounters on the day of presentation.
Goals
Goals for the pilot were outlined in advance and included:
- Significant increase in swing shift physician productivity;
- Complete elimination of non-billable encounters;
- Significant reallocation of advanced practice clinician hours from admitting to rounding;
- Significant reduction in the time between Emergency Department Decision to Admit Order and Hospitalist Admission Order;
- Significant improvement in hospitalist clinician satisfaction scores.
Design
Prior to the pilot, a physician champion was selected and trained in scribe utilization best practices, effective change management and transformational leadership techniques. The physician champion held a series of meetings with participating clinicians and scribes to create shared enthusiasm and team cohesion, outline pilot goals, disseminate scribe utilization best practices, answer questions and address concerns. The physician champion also met with hospital administrators to procure necessary resources and ensure compliance with hospital policies.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As this was non-human-subject research, Institutional Review Board approval was not required. The pilot was conducted over 7 weeks. A week 0 was allotted for medical scribe onboarding, hospital orientation and workflow analysis. Medical scribes staffed weeks 1 and 2 for 8 hours per shift, without any changes to the existing staffing model, in order to allow swing shift physicians to acclimate to scribe utilization. Weeks 3 through 6 were staffed by medical scribes for 12 hours per shift. During weeks 5 and 6, overlapping advanced practice clinician hours were reallocated from admitting to rounding. Data was collected through both quantitative and qualitative measures. Admissions to the hospitalist service were tracked through the electronic health record and billing data. This data allowed us to identify admissions that potentially could have been admitted to a swing shift provider but were passed to another team due to the swing clinician being unable to manage the volume. The electronic health record provided the decision to admit to first order time. Clinician surveys were given both pre- and post-trial to assess their satisfaction and work capacity. Although no other programs were deployed at the same time, the hospitalist team had undergone a recent management change with many new processes implemented that may have continued to improve efficiency. The providers were also aware of the scribe addition to their service and likely suspected more data was being collected than their survey.
Statistical analysis
Qualitative data were obtained via pre-pilot and post-pilot survey. The qualitative results are reported as actual survey responses in the results section, with the percentage changes in pre-pilot vs. post-pilot survey responses highlighted.
Quantitative data were obtained through the measurement of clinician and scribe hours worked, admissions performed, admissions seen or not seen prior to midnight, and throughput intervals. The data were analyzed through descriptive statistics. The quantitative results are reported in the results section.
ROI was calculated by dividing net increased profit per shift by total scribe cost per shift. Net increased profit per shift was calculated as the sum of revenue gained from the capture of the non-billable encounters and improved documentation, plus the savings yielded through the elimination of advanced practice clinician coverage.
Results
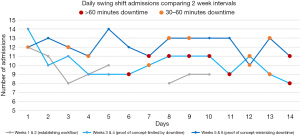
Prior to the pilot, the swing shift admitting physicians were seeing an average of 8.9 admissions per shift. The average admissions per shift increased to 9.6 during weeks 1 and 2, 10.2 during weeks 3 and 4, and 12.2 during weeks 5 and 6 (see Figure 1). Comparing weeks 5 and 6 to the pre-pilot baseline, the pairing of a scribe with the swing shift physician increased the average number of admissions per shift by 3.3, or 37%.
As a result of the increased efficiency, the number of encounters that were not seen before midnight decreased from a pre-pilot average of 4, to an average of 0.5 during weeks 5 and 6 of the pilot. This resulted in an average increase of 3.5 additional billable encounters, an 88% improvement.
During week 6 of the pilot, a total of 7 hours of the advanced practice clinician overlapping coverage (from 11 a.m. to 6 p.m.) was reallocated from admission duties to rounding duties. Despite the subtraction of 7 hours of advanced practice clinician admission capacity, the swing physician was able to maintain productivity and throughput.
The average time from Emergency Department Decision to Admit Order to Hospitalist Admission Order was 38.8 minutes for the swing shift prior to the pilot. By weeks 5 and 6, the average had decreased to 29.8 minutes, an improvement of 23%. The swing shift team’s increased efficiency brought the entire hospitalist team average down from 53.9 minutes pre-pilot to 38 minutes by the end of the pilot, an improvement of 30%. It is notable that the improved swing shift efficiency resulted in greater than additive downstream improvements in overall efficiency. Before the pilot, the nocturnist team often would arrive with multiple patients waiting on Hospitalist Admission Orders who had Emergency Department Decision to Admit orders placed between 6 p.m. and 7 p.m. During weeks 5 and 6 of the pilot, the nocturnist team saw a drop of 15 minutes in their Emergency Department Decision to Admit Order to Hospitalist Admission Order. The day team also saw an impressive 33-minute decrease in their Emergency Department Decision to Admit to Hospitalist Admission Order.
Pre- and post-pilot clinician surveys were conducted. Subjective assessment of perceived workload was also performed on completion of the pilot. Each participating clinician was asked to quantify the number of patients they felt they could comfortably admit per shift, without and with a scribe. Clinician A reported 10 admissions without a scribe and 12 admissions with a scribe (a 25% increase). Clinician B reported 10 admissions without a scribe and 13 admissions with a scribe (a 30% increase).
Both clinicians reported having to stay less than 15 minutes after their shift to complete documentation when paired with a scribe vs. at least an hour without a scribe. Clinician A indicated that the percent of time spent on documentation and other non-clinical tasks decreased from 30% without a scribe to 10% with a scribe. Clinician B noted a respective drop from 50% to 10%. Both clinicians would strongly recommend a scribe to their colleagues and reported fewer symptoms of burnout at work.
Both clinicians stated that scribes helped to improve the thoroughness of their documentation. Clinician A described feeling more energized and experiencing an improved quality of life on his first day off from work. He noted that without a scribe he would typically require a full day off to “recover” from his stretch of blocked shifts. While this clinician initially reported that he typically spent only 15–30 minutes documenting at the end of the shift, the site Medical Director reported that the clinician frequently did so for several hours. When asked why they reported less time on the survey, the clinician noted that they were embarrassed to admit the true time spent in post shift documentation. In addition, several of the ED clinicians subjectively noted a positive change in the overall demeanor of the swing shift admitting clinicians along with quicker pager response times.
Discussion
The medical scribe pilot demonstrated a significant increase in clinician productivity (a 37% improvement). While non-billable encounters were not completely eliminated, the percent reduction was significant (an 88% improvement). A substantial number of advanced practice clinician hours were able to be eliminated from the admitting team (a 58% elimination). The time between Emergency Department Decision to Admit Order and Hospitalist Admission Order was also considerably reduced (a 23% reduction).
Clinician feedback was extremely positive. Job satisfaction for both swing shift team clinicians improved. One clinician noted not only increased daily energy and improved work-life balance, but also a desire to work more shifts if he could continue to utilize a scribe. Daytime hospitalist team clinicians also reported improved morale, sighting the decreased number in spill-over admissions from the ED. Nocturnist job satisfaction also improved due to the reduction in their front-end admission burden. ED clinicians anecdotally noted quicker return of phone calls and improved collaboration with the hospitalist team. We also received reports from hospital staff who stated that they had never seen the hospitalist admission team so happy before. Remarkably, physician burnout relief seems to have extended beyond the single shift to which the scribe partnership was applied.
Despite the clear demonstration of operational and subjective value, medical scribes have a financial cost. In order to determine the ROI for the pilot, the cost of the medical scribes was compared to the revenue gained from the capture of the non-billable encounters and improved documentation, as well as the elimination of the 7 hours of advanced practice clinician coverage. The combined ROI was approximately 322%. The ROI for the additional billable encounters and improved documentation alone was approximately 60%.
This pilot was designed to examine the impact of pairing a medical scribe with a hospitalist physician who was performing serial admissions during a swing shift. There are many barriers to increasing an admitting clinician’s productivity, including patient complexity, availability of medical records, results turnaround time, documentation requirements and myriad other considerations. Removing these obstacles can range from easy to impossible and cost-free to prohibitively expensive. As clinician management groups and hospitals seek to maximize clinician productivity, pairing a medical scribe with a physician who is performing serial admissions should be considered as an option that can simultaneously improve productivity and throughput, while increasing job satisfaction, decreasing burnout risk and producing a ROI. Depending on the size of the program and the particular duties of the shift, such a model could have utility for day, swing and night shifts. Given the higher cost of nocturnist labor, the use case for night shifts is particularly compelling. Finally, in times of surging volumes, such as during the COVID-19 pandemic, deploying a medical scribe could be a cost-effective means of resolving demand capacity mismatches and safeguarding clinician wellness.
The ability of this pilot to demonstrate productivity improvement was constrained by both significant downtime and periods of low volume. During weeks 3 and 4 of the pilot, scribes reported long periods of downtime between admissions, averaging more than 1 hour per day. As this was limiting our ability to demonstrate increased productivity, scribes were asked to report on downtime beginning day 6 of week 3 (see Figure 1). It was subsequently determined that downtime could be reduced by smoothing the timing of admissions (avoidance of batching) from the ED. Prior to the pilot, the ED clinicians had frequently found batching of admissions to be the best way of communicating with the swing shift hospitalist. Admission smoothing, and an enhanced communication plan, was discussed with ED management and downtime subsequently improved in weeks 5 and 6. Downtime, however, did not completely disappear, suggesting that the pilot did not fully realize the opportunity for increased productivity. Figure 1 shows the downtime in relation to admissions completed. A noticeable increase in downtime was not always consistent with low admission days. The hospitalist service also experienced decreased overall volume during the initial weeks of the pilot. Total daily admissions fell by an average of 4.1 per day vs. pre-pilot data between weeks 2 and 4. During the 6 weeks of the pilot, ED volumes were down an average of 11 patients per day vs. trailing 6 weeks of data. In addition, the decreased rounding census caused the well-meaning hospitalist rounding team to assist with admissions, reducing the overall number of admissions available for the swing shift physician. In facilities with continuously unmet demand, it is possible that greater productivity gains could be demonstrated.
Admission complexity was widely variable during the pilot, ranging from uncomplicated observation cases to extremely complicated intensive care unit cases. As complexity increased, the number of admissions performed became an attenuated measure of actual increased productivity. In the future, measuring productivity by relative value unit (RVU) would be an enhancement.
The ability of this pilot to demonstrate productivity was also constrained by its relatively brief duration. It is possible that peak efficiency was not reached during the trial and that greater maturation of the clinician and medical scribe partnership could result in further productivity improvements.
It is also notable that this pilot featured the reallocation of advanced practice clinician hours from admitting to rounding during weeks 5 and 6. This change did introduce potential confounding to the weeks 5 and 6 results, and may have skewed them negatively.
Data collection was precluded on a small number of days by unavoidable scribe vacancies. All data for these dates were removed with the exception of time between the Emergency Department Decision to Admit Order and Hospitalist Admission Orders, the contribution to which was negligible.
The workflow and documentation burden of rounding clinicians is significantly different than that of admitting clinicians. While this pilot demonstrated the efficacy of pairing a medical scribe with an admitting clinician, further study is necessary to determine the potential benefit of pairing a medical scribe with a rounding clinician.
This pilot focused exclusively on pairing a medical scribe with a physician. Further study is also necessary to examine the potential benefit, and associated ROI, of pairing a medical scribe with an advanced practice clinician. ROI validation of scribe utilization could be furthered through tracking revenue generation, reductions in staffing, increased hospital admissions, or clinician turnover (7).
Although this pilot did not sufficiently analyze overall hospitalist throughput metrics and patient satisfaction scores, it is possible that the utilization of medical scribes in the inpatient setting could have benefit to both.
Physician burnout was clearly decreased during the pilot, given the statements provided and satisfaction surveys. Unfortunately, we did not perform a group-wide burnout index prior to the pilot. We suggest that a similar trial with the objective of evaluating physician burnout be performed with utilization of either a Maslach Burnout Index or a Mini-Z burnout assessment (16).
Lastly, in terms of ROI, constrained hospitalist throughput and admission congestion is a common cause of increased ED wait times. If patients are leaving emergency departments without being seen, any measure employed to improve hospitalist throughput, including the use of a hospitalist medical scribe, could have further beneficial impact on ROI.
Conclusions
Pairing a medical scribe with an admitting hospitalist physician led to increased clinician satisfaction, decreased burnout symptoms, and improved productivity. The financial value was demonstrated by a generous ROI. This study suggests that the pairing of a medical scribe with an admitting hospitalist physician can add significantly more value than expense. In the face of surging volume during the COVID-19 pandemic, deploying a medical scribe could be a cost-effective means of resolving demand capacity mismatches and safeguarding clinician wellness.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-26/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-26/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-26/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-26/coif). TeamHealth is a clinician staffing and management company. Dr. MC and Dr. NK are employed by TeamHealth as clinicians and as administrative employees. The pilot was conducted at a facility that where TeamHealth provides clinician staffing and management services. Dr. MC and Dr. NK received no compensation from TeamHealth related to the conduction of the pilot and/or the authorship of this paper. Scribe America providers medical scribes to hospitals and medical practices for a fee. The pilot was conducted at a facility where Scribe America provided medical scribes to TeamHealth clinicians. Ms. CP is employed by Scribe America and received no compensation from Scribe America separate for, or related to, the conduction of the pilot and/or the authorship of this paper.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As this was a non-human-subject research, Institutional Review Board approval was not required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Allred RJ, Ewer S. Improved emergency department patient flow: five years of experience with a scribe system. Ann Emerg Med 1983;12:162-3. [Crossref] [PubMed]
- Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urol 2010;184:258-62. [Crossref] [PubMed]
- Bank AJ, Gage RM. Annual impact of scribes on physician productivity and revenue in a cardiology clinic. Clinicoecon Outcomes Res 2015;7:489-95. [Crossref] [PubMed]
- Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med 2010;17:490-4. [Crossref] [PubMed]
- Bansal A, Bejerano RL, Cashimere CK, et al. Reducing length of stay by using standardized admission process: retrospective analysis of 11,249 patients. Journal of Hospital Medicine 2015;10:abstr 66. Available online: https://shmabstracts.org/abstract/reducing-length-of-stay-by-using-standardized-admission-process-retrospective-analysis-of-11249-patients/ (Accessed September 9, 2020).
- Collins TR. Use of medical scribes spurs debate about costs, difficulties of electronic health records. The Hospitalist, 2015. Available online: https://www.the-hospitalist.org/hospitalist/article/122102/use-medical-scribes-spurs-debate-about-costs-difficulties-electronic (Accessed September 4, 2020).
- Hamzi A, Norman B. An Economic Analysis of Using Scribes to Improve Hospitalists’ Workload. J Hosp Med Manage 2020;6:253.
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 4th ed. Menlo Park: Mind Garden Inc., 2016.
- West CP, Tan AD, Habermann TM, et al. Association of resident fatigue and distress with perceived medical errors. JAMA 2009;302:1294-300. [Crossref] [PubMed]
- Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal Study Evaluating the Association Between Physician Burnout and Changes in Professional Work Effort. Mayo Clin Proc 2016;91:422-31. [Crossref] [PubMed]
- Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA 2018;320:1131-50. [Crossref] [PubMed]
- Gidwani R, Nguyen C, Kofoed A, et al. Impact of Scribes on Physician Satisfaction, Patient Satisfaction, and Charting Efficiency: A Randomized Controlled Trial. Ann Fam Med 2017;15:427-33. [Crossref] [PubMed]
- Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2019;26:106-14. [Crossref] [PubMed]
- Hinami K, Whelan CT, Miller JA, et al. Job characteristics, satisfaction, and burnout across hospitalist practice models. J Hosp Med 2012;7:402-10. [Crossref] [PubMed]
- Gesensway D. Is there a scribe in your future? Today’s Hospitalist, 2018. Available online: https://www.todayshospitalist.com/scribe-in-your-future/
- Olson K, Sinsky C, Rinne ST, et al. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress Health 2019;35:157-75. [Crossref] [PubMed]
Cite this article as: Kesner N, Corvini M, Panter C. Pairing a medical scribe with a hospitalist physician improved clinician satisfaction, increased productivity and provided a return on investment. J Hosp Manag Health Policy 2022;6:38.

