Design, implementation and impact of a new physician role to address capacity challenges at a large academic medical center
Introduction
Hospitals that act as regional referral centers for tertiary and quaternary care are experiencing a growing demand for their services. This demand can place significant strain on inpatient capacity, including beds, personnel, and equipment. Lack of available capacity can delay access to care and threaten the hospital’s ability to provide safe and timely service to patients.
Numerous studies have demonstrated an association between inpatient hospital capacity strain and quality of care indicators, including increased medical errors and mortality (1-3). In addition, waiting times in the emergency department (ED) for admission have been associated with longer length of stay (LOS) and mortality (4-15).
Capacity strained hospitals also experience bottlenecks in shared patient care resources, such as procedural services, radiologic imaging, and specialist consultation (16,17). When these services are overwhelmed by high patient demand they can become a barrier to the advancement of patient care, leading to prolonged LOS which further exacerbates the strain on bed availability.
As demand continues to grow, medical centers are under pressure to increase operational efficiency and facilitate timely access to beds. The Joint Commission, for example, requires hospitals to develop strategies that address the consequences of hospital crowding (18,19). The urgency of developing strategies to address hospital crowding has grown due to the COVID-19 pandemic. The pandemic has created prolonged periods of severe strain on hospital capacity throughout the country, exacerbating pre-existing capacity challenges.
Several aspects of hospital operations that make it difficult for them to address their capacity challenges. First, hospitals are primarily organized into clinical specialties leading to operational silos even though the care pathway of the patient commonly bridges multiple areas. Second, the ability of individuals within one department to advance the care of their patient is limited when progress requires coordination across departments. Typically, coordination across departments requires operational knowledge of the system, organizational relationships and trust with key operators, and bandwidth that may not exist for individuals within each department. As a result, someone with institutionally recognized authority and hospital-wide operational awareness may be needed to help prioritize and coordinate actions across several services.
Several studies have suggested that roles dedicated to actively managing capacity may have a positive impact (20-23). These reports have examined the use of “bed czars” to address capacity challenges, though such roles have often been limited to prioritizing and assigning beds to patients and they have typically not focused on helping with overcoming barriers and bottlenecks to the patient’s progress of care. Further studies are needed to evaluate the design, actions, and impact of roles aimed at improving timely access to care and reducing barriers to patient progress (24,25).
We designed and implemented an institutional role called the Capacity Physician at a large academic medical center with significant capacity challenges. The capacity physician acts as a partner to all clinical and operational services and aims to help address daily capacity challenges with a focus on patient access to care, progress of care during hospitalization, and discharge. We describe the design and implementation of the role and report on the results of a six-month prospective observational period in which we tracked the capacity physician’s consultations, and actions. We present the following article in accordance with the STROBE reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-48/rc).
Methods
Study setting
This study took place at a 1,034-bed quaternary care teaching hospital in Boston, MA. In addition to many service lines, the hospital is a regional center for level one adult and pediatric trauma, burns, stroke, and transplant. In 2019, the hospital had 111,524 ED visits of which 50,434 were admitted and accounted for a total of 332,497 inpatient bed-days. The hospital typically performs more than 36,000 procedures per year.
Intervention
Scope
The capacity physician has hospital-wide scope. She/he works as an advocate on behalf of all care services and in partnership with nursing, physician, and administrative leadership across the institution. The challenges that the Capacity Physician is charged with addressing spans the patient care continuum, including patient access to care (inflow), progress of care during the hospital stay, and discharge (outflow).
Specific aims
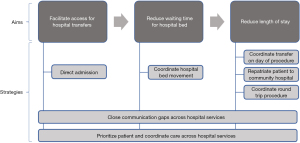
The specific aims of the role for consultations are the following: (I) to increase timely access to care for patients at referring hospitals needing urgent transfer to our quaternary care center; (II) to reduce waiting times for hospital beds for patients in our ED, post-anesthesia care unit (PACU), and other locations; (III) to reduce LOS. A set of strategies that were designed to be used by the Capacity Physician to achieve these aims are outlined in Figure 1. Table 1 provides a description of each strategy.
Table 1
| Strategies | Description |
|---|---|
| Direct admission | Facilitate patient transfer from the ED of a referring hospital by admitting the patient directly to an inpatient location (general care ward, ICU, or procedural space) |
| Coordinate hospital bed movement | Facilitate patient access to an inpatient bed by coordinating movement of patients between beds across different departments |
| Coordinate transfer on day of procedure | For appropriate patients from a referring hospital needing a procedure, work with the referring hospital to time the transfer of a patient on the day of procedure |
| Repatriate patient to community hospital | For appropriate patients who were transferred from a referring hospital, work with case management to transfer the patient back to the referring hospital after the tertiary portion of care is completed |
| Coordinate round trip procedure | For appropriate patients from a referring hospital needing a specific procedure, facilitate transfer of the patient back to the referring hospital immediately after post-procedural anesthesia recovery |
| Close communication gaps across hospital services | Coordinate across departments when there is a lack of communication that is delaying care |
| Prioritize patient and coordinate care across hospital service | For patients with urgent care needs, work with hospital services to prioritize the patient’s care and help coordinate delivery of services |
ED, emergency department; ICU, intensive care unit.
Role and responsibilities
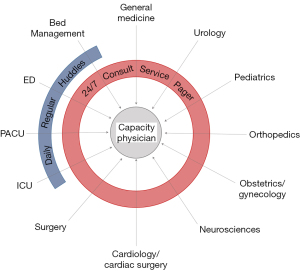
The capacity physician is responsible for monitoring the daily capacity situation across the hospital in order to maintain situational awareness of challenges. As illustrated in Figure 2, the capacity physician is responsible for addressing challenges that come to its attention through daily touchpoints with key care services and via a consultation pager system with 24/7 availability. The capacity physician reports directly to senior hospital administrative leadership. She/he is on-site at the hospital five days per week during daytime hours and is immediately available via pager when off-site during nighttime and weekend hours. Five physicians from multiple specialty backgrounds rotate through the role on a seven-day rolling basis.
Qualifications
The capacity physician is a clinically trained individual who maintains an active clinical practice outside of his or her duties as capacity physician. The capacity physician must have experience in operational leadership within the hospital. When serving in the role, she/he is required to work without bias toward a specific care service or department. She/he must be able to communicate effectively across care services, understand how to coordinate in a collaborative fashion, and develop trust with different role groups and service areas throughout the institution. Clinical background was deemed necessary for the role given that many capacity operations decisions involve clinical triage, prioritizations, weighing different clinical options and pathways, and communicating, guiding, and sometimes negotiating with clinician decision-makers throughout the hospital (especially attending physicians).
Recruitment
The capacity physicians were recruited by the program (authors KS and PD) among the hospital’s physicians with existing clinical-operational leadership roles. Those selected had existing roles within the emergency department, inpatient general medicine, critical care, and procedural services. Given the diversity of clinical-operational experience of this group, capacity physicians were encouraged to share operational knowledge across team members and use each other as resources when on-call. Time spent covering the capacity physician role was integrated within the existing administrative time that these individuals possessed within their schedules. The role was funded by the hospital and each clinical department to which the capacity physicians belonged.
Training
The leaders of the capacity physician program created a training manual to help orient capacity physicians to the role. The manual included: an overview of the scope, aims, and expectations of the role; a schedule of required capacity-related operational huddles occurring throughout the day, their aims, and the capacity physicians role; a list of common capacity-related challenges and potential levers to help resolve these issues; and a list of key contacts in various clinical and operational realms related to capacity. A monthly debrief meeting was implemented to review challenging cases and gather feedback to improve the role, which was used to expand and enrich the guidance manual.
Descriptive outcomes
We prospectively tracked the consultations, actions, and impact of the capacity physician from its implementation on September 9, 2019 through January 31, 2020. Data collection and the use of data for this analysis was approved by the institutional review board (IRB) of Partners Healthcare, Boston, MA, USA (institutional review board protocol 2011P01124). Participant consent was waived as this was performed as a quality improvement study, for which our IRB does not require informed consent of participants. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
We tracked the total volume of consultations received during the study period and the average volume of consultations per week. The volume of consultations received was tracked using a time-stamped log of pages in the hospital paging directory and via daily email-based survey of individuals serving in the role. The date of the request and the name of the originating service of the consultation were recorded.
For each consultation, the Capacity Physician reported on the capacity challenge for which they were consulted and these were categorized by a member of the study team based upon six common themes: (I) ED at critical capacity level; (II) PACU at critical capacity level; (III) ICU at critical capacity level; (IV) general care at critical capacity level; (V) communication/coordination gap across care services causing delay in care; (VI) discharge-dependent care service delay. A single consultation could be attributed to more than one theme.
In addition, for each consultation the Capacity Physician reported the actions that she/he took to address the challenge. These were categorized by a member of the study team into one of the seven strategies listed in Figure 1.
Finally, for each consultation the Capacity Physician reported the outcome of the consultation on capacity. These were attributed to one of the three aims listed in Figure 1 by a member of the study team.
Results
The capacity physician received 155 consult requests during the study period, representing 7.2 consults per week. Figure 3 demonstrates the number of consult requests by location or department. Overall, 14 locations or departments requested consultation. The largest proportion originated from the general medicine and general surgery departments, accounting for 51.6% of all requests.
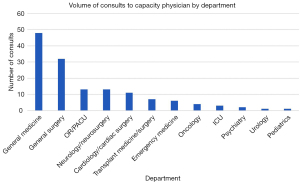
Table 2 demonstrates the most common capacity challenges for which consultation was requested, the actions taken by the capacity physician to address the challenge, and the impact on the hospital. The most common challenges encountered were critical capacity levels in the ED (44, 28.4%), communication/coordination gaps across clinical services (37, 23.9%), and critical capacity levels in the general care wards (29, 18.7%). The most common action taken by the capacity physician during consultation was to prioritize a patient and help coordinate their care across services (54, 34.8%). The most common impact on capacity as a result of the consultation was reduced LOS (78, 50.3%).
Table 2
| Category | Subcategory | Number of consults | % of consults |
|---|---|---|---|
| Capacity challenge | ED without capacity | 44 | 26.7% |
| Care delay caused by communication/coordination gap across hospital services | 37 | 22.4% | |
| General care wards without capacity | 39 | 23.6% | |
| Discharge-dependent hospital service delay | 23 | 13.9% | |
| PACU without capacity | 12 | 7.3% | |
| ICU without capacity | 10 | 6.1% | |
| Strategy used | Prioritized patient and coordinated care across hospital services | 54 | 34.8% |
| Direct admission | 30 | 19.4% | |
| Coordinated hospital bed movement | 30 | 19.4% | |
| Closed communication gaps across hospital services | 27 | 17.4% | |
| Coordinated transfer on day of procedure | 8 | 5.2% | |
| Repatriated patient to community hospital | 4 | 2.6% | |
| Coordinated round trip procedure | 2 | 1.3% | |
| Outcome | Reduced length of stay | 78 | 50.3% |
| Facilitated access for hospital transfer | 46 | 29.7% | |
| Reduced waiting time for hospital bed | 31 | 20.0% |
ED, emergency department; PACU, post anesthesia care unit; ICU, intensive care unit.
The departments that most often were impacted included the following: emergency department 51 (24.8%), general medicine 49 (23.8%), general surgery 34 (16.5%), operating room/post anesthesia care unit 18 (8.7%), cardiology/cardiac surgery 13 (6.3%), neurology/neurosurgery 12 (5.8%), orthopedics 10 (4.9%), transplant medicine/surgery 6 (2.9%), oncology 4 (1.9%), psychiatry 3 (1.5%), ICU 3 (1.5%), urology 2 (1.0%), and gynecology 1 (0.5%).
Discussion
At a large quaternary care hospital, we designed and implemented a new role called the Capacity Physician that acted as a 24/7 consultation resource to help address barriers to patient access, progress of care, and discharge. Over a 5-month period, the Capacity Physician was consulted 155 times by 14 different services. We found that the most common reasons for consultation were related to ED and general care ward capacity, communication/coordination gaps across multiple clinical services, and discharge-dependent service delays. Capacity Physicians reported using several strategies during consultations, the most frequent of which was helping to prioritize a patient and coordinate care across services in the hospital. The impact of consultations that we observed included facilitation of urgent patient access to the hospital, reduction of LOS, and decreased waiting time for inpatient beds.
This study adds to the literature on hospital-wide interventions aimed at increasing the coordination of inpatient capacity operations. Another large academic medical center reported on the design and implementation of a capacity command center that coordinated patient access and flow throughout the system by collocating teams, offering visual displays of current capacity scenarios, and building standard protocols to aid in patient flow (20). Early evidence indicated that such a cross-institutional function could be helpful in reducing delays in patient care. We believe that our study expands upon this work by describing how a physician leadership role with a similar focus could be used to impact capacity.
We observed several themes in successful consultations performed by the capacity physician. First, the capacity physician was able to identify patients who needed prioritization and ensure that they gained access to our hospital’s services in a timely fashion. These were often patients at referring hospitals with quaternary care needs whose transfer was delayed or at risk of being denied due to capacity challenges, particularly in the ED. Common patient populations in this category included major traumas, solid organ transplant candidates, burns, aortic emergencies, and new brain tumors. Frontline access nurses and physicians clinically accepting these patients onto their service could consult the capacity physician for help. Working with other operational role groups, the capacity physician used alternative methods to accommodate patients in a timely fashion, such as direct admission to an appropriate inpatient location such as a general care ward, ICU, or procedural suite, thus bypassing the crowded emergency department.
Another area of success was eliminating barriers to progress of care and discharge. These consultations often originated from care teams on the hospital’s general care wards. Common examples included delays in interventional radiology procedures that represented the final milestone of care in preparation for discharge to home or transition to a post-acute facility. Common procedures included the placement of percutaneous gastrostomy tubes, peripherally inserted central catheters, and dialysis access lines. In many cases, we found that the care teams did not have a clear understanding of why the service was delayed and did not know who to contact to advocate for greater prioritization. On the other hand, proceduralists voiced challenges in perceiving when their service was a bottleneck. Critical to the capacity physician’s success was establishing a strong operational knowledge of how the system worked and with whom to coordinate to reprioritize patients. By repeatedly working with operational leads from these services, the capacity physician was able to establish trust.
We found that several aspects of the way that the capacity physician role was designed were critical to its success. First, in order to establish a strong situational awareness of rapidly evolving capacity challenges, it was essential for the capacity physician to be integrated within the operational structure of daily hospital capacity management. This included regular, standard huddles during the day with operational leaders from bed management and clinical triage from the general care, ICU, procedural, and ED services. These huddles were frequently a source of consultation with the capacity physician as well. Another helpful tool to establishing continual situational awareness of the hospital’s capacity challenges was a hospital-wide dashboard that provided transparency into bed availability and queuing in key areas, including inpatient, ED, PACU, and outside hospital transfers.
We also found that key characteristics of individuals serving in the capacity physician role were instrumental to its success. One of these was the ability to act in a role that served all clinicians and services within the hospital without bias. Frequently the capacity physician role required bridging communication gaps across different departments and finding a way to frame challenges in a way that helped resolve disagreements. We also found that the diverse clinical backgrounds of the individuals serving in the role, including medicine, surgery, critical care, and ED, was an asset. Each person had unique expertise in the operational intricacies of their home care environment and could help support each other’s learning of different care environments that they were less familiar with.
We also found that many of the consultations that the capacity physician received centered around common challenges for which standardized processes could be developed. Through standardization, we could ensure that the capacity physician was consulted early on and that the coordination with other key role groups could be more efficient. For example, we standardized a direct admission pathway during periods of extreme ED congestion such that the capacity physician was automatically paged along with other key operational leaders immediately.
After the study period, the capacity physician continued to evolve within the institution. The role, which was established approximately six months prior to the pandemic, was a critical part of the hospital’s COVID-19 response. The hospital experienced a severe wave of COVID admissions during the Spring 2020 with numerous surge ICUs opened and general care units repurposed for COVID care. The capacity physicians attended daily hospital incident commands system meetings and were asked to help guide units on patient flow in collaboration with other leading clinical-operational roles throughout the hospital. This was especially important because the clinical triage guidelines of the hospital evolved rapidly and substantially during this period. Services admitted COVID and other diagnoses that they historically did not manage. In addition, the types of critical care patients that the surge ICUs could admit were limited and the traditional ICUs were required to expand and sometimes contract the typical populations that they would admit. The capacity physician played an important role in helping ICU staff navigating these changes. The role also helped to administer inpatient transfer criteria for COVID patients throughout the pandemic, ensuring that those brought to our quaternary care center were appropriate given that hospital capacity was so limited and needed to carefully manage its precious beds to ensure availability for the sickest patients in the region (e.g., COVID requiring extra corporeal membrane oxygenation (ECMO).
In addition, the role was integrated within a new capacity coordination center, which the hospital opened in August 2020. The center houses key operational role groups noted in Figure 1, which are critical to help coordinate and support efficient patient inflow, progress of care and outflow throughout the hospital. Prior to the center, the physical separation of these role groups from each other and the capacity physician was a barrier to efficient communication. Communications typically occurred via individual phone calls, group emails, or text messages, which were at times redundant and difficult to coordinate. Early experience of the capacity physician in the center indicates that these barriers have been reduced and communication is more continuous throughout the day.
An important limitation of our study is that we did not record details regarding cases in which the capacity physician was consulted but could not make an impact. Certain capacity challenges were not solvable in the role and often represented significant limits of the current system that required longitudinal solutions. Examples raised included the need for additional licensed beds, expanded treatment spaces in the ED, and additional resources particularly at nights on and on weekends. We were also limited in our ability to analyze aggregate measures in hospital capacity related to the role. The capacity physician role addressed non-standard, complex patient access and flow scenarios and therefore aggregate measures of impact on capacity, such as LOS or ED waiting times, are unlikely to be significantly changed. Another limitation of our study is that it occurred at a single center and it is unclear whether the capacity physician could be scaled and its impact generalized to other hospitals. While our study may be a helpful building block for other hospitals, it is important to note that the bottlenecks and challenges in their institution may be unique. Critical aspects of the program that could serve as significant barriers at other hospitals include gaining institutional support from senior leadership to fund and establish the role and filling it with individuals who are operationally experienced and trusted within the institution to work across silos. In addition, the success of the capacity physician role is also highly dependent on successful collaboration with effective co-leads in nursing and administration with a similar hospital-wide scope and focus on operations.
Conclusions
An institutional role called the capacity physician was designed to improve patient access, progress of care, and discharge by working across operating silos within the hospital. At an academic medical center with substantial capacity challenges, the role was successfully implemented and utilized by a large number of departments. Several themes emerged in terms of the strategies used by the capacity physician to successfully resolve challenges and the role was successful in impacting patient access, waiting times for beds, and LOS. The capacity physician represents a novel approach that hospitals should consider as they search for strategies to address the significant quality and safety challenges caused by capacity strain and crowding.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-48/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-48/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-48/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-48/coif). WCL receives royalty payment for intellectual property/patent license from Codonics with payment split per institutional policy (hospital, department, lab, inventor) and holds ownership of software company EasyCV LLC that curates medical school CV data and CV formatting. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Participant consent was waived as this was performed as a quality improvement study, for which our IRB does not require informed consent of participants. Data collection and the use of data for this analysis was approved by the institutional review board (IRB) of Partners Healthcare, Boston, MA (institutional review board protocol 2011P01124). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Madsen F, Ladelund S, Linneberg A. High levels of bed occupancy associated with increased inpatient and thirty-day hospital mortality in Denmark. Health Aff (Millwood) 2014;33:1236-44. [Crossref] [PubMed]
- Abir M, Goldstick J, Malsberger R, et al. The Association Between Hospital Occupancy and Mortality Among Medicare Patients. Jt Comm J Qual Patient Saf 2020;46:506-15. [Crossref] [PubMed]
- Volpe FM, Magalhães AC, Rocha AR. High bed occupancy rates: Are they a risk for patients and staff? Int J Evid Based Healthc 2013;11:312-6. [Crossref] [PubMed]
- Moskop JC, Sklar DP, Geiderman JM, et al. Emergency department crowding, part 1--concept, causes, and moral consequences. Ann Emerg Med 2009;53:605-11. [Crossref] [PubMed]
- Rabin E, Kocher K, McClelland M, et al. Solutions to emergency department 'boarding' and crowding are underused and may need to be legislated. Health Aff (Millwood) 2012;31:1757-66. [Crossref] [PubMed]
- American College of Emergency Physicians: Policy Statement: Crowding. Accessed Dec 14, 2018. Available online: https://www.acep.org/globalassets/new-pdfs/policy-statements/crowding.pdf
- Institute of Medicine: Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press, 2006.
- Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med 2008;52:126-36. [Crossref] [PubMed]
- Singer AJ, Thode HC Jr, Viccellio P, et al. The association between length of emergency department boarding and mortality. Acad Emerg Med 2011;18:1324-9. [Crossref] [PubMed]
- Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med 2013;61:605-611.e6. [Crossref] [PubMed]
- Pines JM, Iyer S, Disbot M, et al. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med 2008;15:825-31. [Crossref] [PubMed]
- Fordyce J, Blank FS, Pekow P, et al. Errors in a busy emergency department. Ann Emerg Med 2003;42:324-33. [Crossref] [PubMed]
- McGowan JE, Truwit JD, Cipriano P, et al. Operating room efficiency and hospital capacity: factors affecting operating room use during maximum hospital census. J Am Coll Surg 2007;204:865-71; discussion 871-2. [Crossref] [PubMed]
- Chalfin DB, Trzeciak S, Likourezos A, et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 2007;35:1477-83. [Crossref] [PubMed]
- Harris S, Singer M, Rowan K, et al. Delay to admission to critical care and mortality among deteriorating ward patients in UK hospitals: a multicentre, prospective, observational cohort study. Lancet 2015;385:S40. [Crossref] [PubMed]
- Cournane S, Conway R, Creagh D, et al. Radiology imaging delays as independent predictors of length of hospital stay for emergency medical admissions. Clin Radiol 2016;71:912-8. [Crossref] [PubMed]
- Rahman AS, Shi S, Meza PK, et al. Waiting it out: consultation delays prolong in-patient length of stay. Postgrad Med J 2019;95:1-5. [Crossref] [PubMed]
- Wiler JL, Welch S, Pines J, et al. Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus summit. Acad Emerg Med 2015;22:542-53. [Crossref] [PubMed]
- McHugh M, Van Dyke K, McClelland M, et al. Improving Patient Flow and Reducing Emergency Department Crowding: A Guide for Hospitals. Agency for Healthcare Research and Quality Oct 2011; AHRQ Publication No. 11(12)-0094. Accessed Oct 11, 2018. Available online: https://www.ahrq.gov/sites/default/files/publications/files/ptflowguide.pdf
- Kane EM, Scheulen JJ, Püttgen A, et al. Use of Systems Engineering to Design a Hospital Command Center. Jt Comm J Qual Patient Saf 2019;45:370-9. [Crossref] [PubMed]
- Howell E, Bessman E, Kravet S, et al. Active bed management by hospitalists and emergency department throughput. Ann Intern Med 2008;149:804-11. [Crossref] [PubMed]
- Chang AM, Cohen DJ, Lin A, et al. Hospital Strategies for Reducing Emergency Department Crowding: A Mixed-Methods Study. Ann Emerg Med 2018;71:497-505.e4. [Crossref] [PubMed]
- Geer R, Smith J. Strategies to take hospitals off (revenue) diversion. Healthc Financ Manage 2004;58:70-4. [PubMed]
- National Academy of Engineering; Institute of Medicine: Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington, DC: National Academies Press, 2005.
- President's Council of Advisors on Science and Technology: Better Health Care and Lower Costs: Accelerating Improvement Through Systems Engineering. Accessed Dec 14, 2018. Available online: https://obamawhitehouse.archives.gov/sites/default/files/microsites/ostp/systems_engineering_and_healthcare.pdf
Cite this article as: Safavi KC, Bravard MA, Yun BJ, Levine WC, Dunn PF. Design, implementation and impact of a new physician role to address capacity challenges at a large academic medical center. J Hosp Manag Health Policy 2022;6:17.