Hospital policy following cancelled orthopaedic surgery and the patient experience—making the best of a bad situation
Introduction
As access to information and news regarding healthcare inflates, maintaining a high standard of communication between surgeons and patients has become a key factor in safeguarding the patient experience (1). Over the last decade there has been a notable national increase in the number of scheduled elective surgical procedures from 6.3 million to 7.9 million in 2017. During this period there has been a disproportionate increased number of cancelled elective cases, rising from 55,209 to 80,572 (2). A cancellation on the day of surgery can be especially frustrating for patients having mentally prepared and incurring significant personal financial burden from being re-listed. Improving the patient experience via communication is beneficial in such scenarios as it: improves doctor-patient relationships and patient perception of control over their care, increased tolerability of pain and some research even indicates reduced length of hospital stay following surgery and therefore reduced cost of care (3-5). Effective communication can also benefit doctors; by satisfying patients and meeting their expectations there is reduced likelihood of patient complaints (6). This reduces work related stress due to litigation proceedings and offers better job satisfaction from positive personal feedback and interaction.
Due to increasing strains on surgical services and staffing levels, patients are regularly not formally apprised of cancellations by doctors and sent home without clarity of their treatment plan (7). This is commonplace despite national guidelines from the Association of Anaesthetists of Great Britain and Ireland (AAGBI) theatre efficiency document in 2003 defining standards of practice in the event of a cancelled operation for non-clinical reasons as outlined in Table 1 (8). The guidance outlines the patient’s right to a timely apology and explanation by a senior member of the team, provision of something to eat and drink as well as organisation of a revised date for surgery within 28 days.
Table 1
| AAGBI Theatre Efficiency Guidance |
| Following a cancellation of surgery, a senior member of the team should visit the patient as soon as possible and offer an appropriate apology and an explanation |
| The patient must be offered another binding date for surgery within a maximum of the next 28 days |
| The patient should be provided with something to eat and drink as soon as possible |
| Patients should be provided with access to a telephone and offered help with arrangements for transport home if appropriate |
To the best of our knowledge no study has assessed the patient experience surrounding cancelled cases within elective orthopaedics. This study aimed to assess our unit’s ability to adhere to the national guidance in the context of cancelled cases on the day of surgery and the subsequent impact on patient satisfaction and understanding regarding their care.
Methods
A prospective study was designed utilising survey data regarding communication and patient perceptions of care surrounding cancelled elective orthopaedic cases in the last 12 months. A total of 126 patients were shortlisted as meeting the inclusion criteria as having a cancelled elective orthopaedic procedure on the day of surgery in a dedicated elective orthopaedic unit for non-clinical reasons. A cancellation was defined as per NHS England guidance: a cancelled procedure on the day of surgery or admission which is not re-listed with completion of surgery within 24 hours. Inclusion criteria outlined patients: to be older than 16 years of age, having an abbreviated mental test score (AMTS) >9 and being able to fully complete the survey independently.
Of the 126 patients, 1 was removed for being incorrectly logged as a cancellation. On examining theatre schedules this patient was re-listed and had surgery the following day (thus meeting the criteria for a postponement rather than a cancellation). A further 4 patients were not contactable and 4 opted not to take part when gaining informed consent producing a final cohort size of 117. All participants in the final cohort gave informed consent prior to taking part in the study.
All patients were surveyed following re-listing via a survey assessing: which type of healthcare professional notified them of the cancellation (e.g., consultant, junior doctor, nurse, other); if sufficient time was allocated to fully explain the reasoning to them; patient level of understanding and satisfaction with the reason for cancellation out of 10 and perception of being kept nil by mouth (NBM) longer than necessary. Patients were also asked their opinion on the ideal healthcare professional to inform them of a cancellation, if they were offered formal access to a telephone and if they felt help was available for transport home if needed. Individuals were allowed to take as long as needed to complete the survey without a healthcare professional present. Theatre schedules were studied to assess the number of days taken to re-list patients. These questions looked to assess the unit’s adherence to cancellation of surgery for non-clinical reasons guidance outlined in the AAGBI theatre efficiency guidelines.
A two-tailed t-test was employed to generate P values in order to assess patient understanding and satisfaction scores. Data was presumed significant at P<0.05. Ethics approval was not warranted for the study being that and no changes were made to the current practice of staff or management protocols within the unit but rather an assessment was being made in comparison to national guidelines.
Results
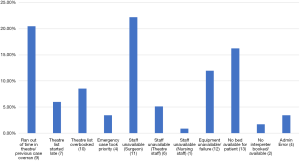
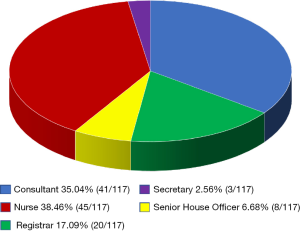
A total of 117 patients were surveyed regarding their cancellations comprising of 62 females and 54 males with an average age of 54 years old (range, 18–85 years old). The top 3 reasons for cancellations were a surgeon not being available (22.22%), theatre sessions overrunning (20.50%) and no bed being available for the patient (16.24%). Breakdown of causes of cancellation are outlined in Figure 1. Sixty-nine patients (58.97%) were informed of their cancellation by a doctor, 45 patients (38.46%) by nurses and 3 patients (2.56%) by surgical secretaries as outlined in Figure 2. Of those informed by doctors: 41 patients (35.04%) were informed by a consultant, 20 patients (17.09%) by a registrar and 8 patients (6.84%) by a senior house officer (SHO); 36 patients (30.77%) felt they were not given adequate time by the healthcare professional informing them regarding the cancellation.
Overall, the average understanding out of 10 was 6.86 (SD ±1.67) and satisfaction 5.23 (SD ±1.82) with a full breakdown between different professionals noted in Table 2. The 41 patients informed by consultants had an understanding score of 8.31 (SD ±0.96) and satisfaction score of 6.37 (SD ±1.73). This is compared with the 45 patients apprised of cancellations by nurses where understanding of information was 5.12 (SD ±1.18) and satisfaction with the reason was 4.07 (SD ±1.42). Two-tailed t-tests revealed a significant difference between nurses and consultants regarding patient understanding and satisfaction scores where statistical analysis indicated P<0.001.
Table 2
| Healthcare professional | Mean patient understanding | Mean patient satisfaction |
|---|---|---|
| Consultant | 8.31 (SD ±0.96) | 6.37 (SD ±1.73) |
| Registrar | 7.40 (SD ±0.98) | 5.95 (SD ±1.61) |
| SHO | 7.00 (SD ±0.78) | 4.50 (SD ±0.97) |
| Nurse | 5.12 (SD ±1.18) | 4.07 (SD ±1.42) |
| Secretary | 3.50 (SD ±0.50) | 2.50 (SD ±0.50) |
SHO, Senior House Officer.
When asked who the ideal healthcare professional was to inform patients of cancellations, 106 patients (90.60%) felt a consultant was best suited however 83 patients (70.94%) stated they would have been satisfied with a registrar. Furthermore, 27 patients (23.08%) stated they would have been satisfied if notified by a nurse; 41 patients (35.04%) perceived they were kept NBM longer than necessary. Frequency of patients feeling they were NBM too long was higher with individuals informed by nurses 60% (27/45) compared to those told by doctors 20.29% (14/69).
One hundred and fifteen patients (98.29%) were offered a new date for surgery within 28 days with completion of their procedure at an average of 17.31 days; 2 patients (1.71%) were mis-informed of their original surgery re-list within 28 days. They were subsequently re-listed at day 30 and 56; 59 patients (50.43%) were offered formal access to a telephone and 55 patients (47.00%) felt there was transport help available if needed to get home.
Discussion
Effective and consistent communication are cornerstones of modern surgical care. The General Medical Council outlines domains for communication and its importance in establishing patient partnerships as part of Good Medical Practice (14). There is an increasing need to adhere to these principles at a time when medical information is easily accessible via news articles and social media platforms. Availability of unfiltered and non-substantiated information means patients can be misinformed and have concerns regarding their care (10). Doctors are best suited to provide patient centred information and tailor the discussion to individual needs and concerns. Our study noted only 58.97% of patients were informed of their cancellation by a doctor. Sub-standard communication risks patient concerns remaining unalleviated and has a detrimental impact on: anxiety levels, mental wellbeing, ability to manage pain, physiological status and can collectively impact on length of stay in hospital (15). O’Connor et al. noted tailored pre-operative information for arthroplasty patients corresponded with improved generalised anxiety disorder scores which is known to correlate positively with intensity and chronicity of post-operative pain (16). Miscommunication also creates a lack of clarity or deliverance of key guidance regarding being re-listed to avoid further cancellations and potentially treatment failure. The outcome is inefficiency in our service with: lost theatre time, poor allocation of bed space and wasted provisioned resources including healthcare staff (17).
One method to diminish these costs is ensuring a senior member of the surgical team informs patients of cancellations in a timely manner as outlined in the AAGBI guidance (8). From our study 38.46% of patients were informed by nurses yet only 23.08% of patients stated they would be satisfied by a nurse led explanation. Nurses are essential to ensure care plans are delivered and patient concerns are escalated. Junior doctors working in surgery are increasingly busy and often do not fully understand reasons why a patient may have been cancelled—equally, given that it is unlikely that they would be in theatre for that procedure, patients can feel dissatisfied that they are not seeing the consultant or registrar involved in their care (12). Ferguson et al. noted that SHOs could not be asked to further increase their level of activity in a study assessing the out of hours workload of surgical junior doctors and that additional staff was required to maintain a high standard of care (18). With ongoing medical rota gaps, nursing staff have unwittingly become the modern mediators of communication between physicians and patients (19). However, being ward based professionals, nurses may not have sufficient knowledge surrounding the reasons for a cancellation of surgery or the communication training and experience to deliver bad news in a comprehensive way. Manner in which information is disseminated to patients improves level of understanding and retention of information which in turn enhances compliance to care plans (20). Furthermore, after having your operation cancelled, the key question is when the patient will be re-listed—often nurses may not know that answer to this, which again can heighten anxiety and frustration. This is indicated by the significantly lower satisfaction scores out of 10 with those patients informed by nurses (5.12) compared to those informed by consultants (6.37).
There was lower standard deviation in understanding scores in the consultant data (SD ±0.96) compared to the nursing group (SD ±1.18). Modern medical schooling and subsequent surgical training pathways fosters development of robust communication skills over time (21). This is further corroborated by the fact that the registrar understanding scores standard deviation was similar to consultants at (SD ±0.98). Upon reaching consultancy, a practitioner should be competent to deliver bad news to patients in a variety of settings which underpins the reason for the comparatively more uniform dataset in this group (13).
Tighter strain on budgets has stretched surgical services in the current climate and has meant practitioners have less time to allocate per patient as their workloads intensifies (22). This problem has exacerbated significantly in the last decade despite the number of doctors per patients rising five times faster than the UK population since 1960 (23). However, when scrutinising the number of specialist surgical service professionals, we note as of 2014 there was only 7,285 consultants working in the public sector (24). This number has remained quite static despite a 27% national increase in admissions for surgical procedures between 2004 to 2014 (25). It is therefore becoming more challenging to offer a satisfactory senior led inpatient surgical experience. It is of no surprise that 30.77% of patients in the study felt they were not given adequate time to discuss the ramifications of their cancellation. The AAGBI guidance states that a senior member of the team should attend to the patient and offer an apology and explanation for a cancellation (8). However, the understanding of what defines a senior team member is left open to interpretation. Consultants are a finite resource with diverse responsibilities and therefore may be unavailable to offer support to an acutely arising cancellation despite our data suggesting 90.60% of patients favoured them as the ideal professional to discuss a cancellation (9). Patient’s may feel they are not being afforded an environment to voice their concerns, discouraging them from requesting more information where needed leading to treatments target not being achieved (26). A realistic alternative to guidance suggesting consultants leading all such conversations or a clearer outline of the definition of a senior team may need to be sought.
The hierarchical system amongst junior doctors places significant value on registrars and the vital role they play in delivering care and maintaining patient safety. Registrars are often perceived to be senior members of a surgical team by healthcare practitioners and patients alike (11). In the context of a cancellation a senior registrar would often have the experience to establish a patient’s needs and concerns as well as respond with a clear tailored plan for the patient to be competently re-listed in a timely manner (27). 70.94% of patients in this study agreed they would have been satisfied if informed of their surgical plan by registrars. It can be suggested that consultants where possible could offer a registrar led explanation if they are unable to do so themselves provided the registrar has the necessary experience required to lead such a discussion. Should patients remain unsatisfied a consultant discussion could still be sought prior to discharge. This is not a current standard in the guidance despite registrar led discussions meeting patient expectations. By having a senior member of the team attend in advance you reduce the likelihood of patients being kept NBM longer than needed as the registrar facilitates care with the ward-based team. Interestingly our study noted 35.04% of patients perceived they were kept NBM longer than needed. It appears nurses in our study informing patients of cancellations remained hesitant to remove the NBM status immediately compared with those informed by doctors. Nursing staff may not be well versed of the situation in theatres. As such nurses may be cautious to withdraw NBM status on the chance that an alternative plan was being formulated to organise surgery for these patients later in the day. By having a registrar attended as early as possible it clarifies the patients care plan and avoids the detrimental impact of keeping patients starved longer than needed (28).
One limitation of our study was our site of testing being an elective unit. Considering how our service is run, theatre lists are often not adjusted for urgent cases as would occur in hospitals accepting acute trauma where patients are at home awaiting surgery on an emergency list (17). Therefore, it is reasonable to assume due to the higher number of cancellations in tertiary trauma centres a greater proportion of patients may be informed of cancellations by nurses, secretaries and non-medical staff via phone which is less than satisfactory. This was notably the case in Mehta et al. which noted in the acute orthopaedic setting 54.7% of patients were informed of cancellations by nurses with no formal communication at all in a further 13.3% (29). Poor communication means patients remain unclear of their subsequent treatment plan, creating a potential for wastage of theatre time and financial loss for the NHS.
Conclusions
It is deeply distressing to experience a cancelled elective procedure on the day of one’s surgery as well as wasteful of stretched NHS resources. Peri-operative interaction between surgeon and patient has a significant effect on overall experience and paves the way for successful relisting to curtail this burden. Improving access to a senior surgeon who can orchestrate this process as well as modifying national guidelines to meet patient’s expectations is central to safeguard individuals during this period and avoid wastage of already stretched resources. It is paramount guidelines exist such that patients are informed of reasons for cancellation by a senior surgeon and their prospective care plan in a timely manner.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jhmhp.2018.10.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was not warranted for the study being that and no changes were made to the current practice of staff or management protocols within the unit but rather an assessment was being made in comparison to national guidelines. Written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Househ M, Borycki E, Kushniruk A. Empowering patients through social media: The benefits and challenges. Health Informatics J 2014;20:50-8. [Crossref] [PubMed]
- NHS Digital. Hospital Episode Statistics, Admitted Patient Care, England, 2013–2014. Available online: https://www.digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/hospital-episode-statistics-admitted-patient-care-england-2013-14#section-resources
- Simpson M, Buckman R, Stewart M, et al. Doctor-patient communication: the Toronto consensus statement. BMJ 1991;303:1385-87. [Crossref] [PubMed]
- Maguire P, Pitceathly C. Key communication skills and how to acquire them. BMJ 2002;325:697-700. [Crossref] [PubMed]
- Stewart M, Brown J B, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract 2000;49:796-804. [PubMed]
- Tongue JR, Epps HR, Forese LL. Communication skills for patient-centered care: research-based, easily learned techniques for medical interviews that benefit orthopaedic surgeons and their patients. J Bone Joint Surg Am 2005;87:652-8. [Crossref]
- Pincock S. Poor communication lies at heart of NHS complaints, says ombudsman. BMJ 2004;328:10. [Crossref]
- The Association of Anaesthetists of Great Britain and Ireland. Theatre Efficiency: safety, quality of care and optimal use of resources 2003. Available online: http: //www.aagbi.org/publications/guidelines/theatre-efficiency
- Sharma A, Sharp D, Walker L, et al. Stress and burnout in colorectal and vascular surgical consultants working in the UK National Health Service. Psychooncology 2008;17:570-6. [Crossref] [PubMed]
- Blake JH, Schwemmer MK, Sade RM. The Patient-Surgeon Relationship in the Cyber Era. Thoracic Surgery Clinics 2012;22:531-8. [Crossref] [PubMed]
- Medford AR. Service contribution and cost-effectiveness of specialist registrars in NHS trusts: a survey and costing analysis. Clin Med (Lond) 2016;16:607. [Crossref] [PubMed]
- Rimmer A. Junior doctors’ low morale is putting patients at risk, Royal College of Physicians warns. BMJ 2016;355:i6493. [Crossref] [PubMed]
- Wouda JC, van de Wiel H. The communication competency of medical students, residents and consultants. Patient Educ Couns 2012;86:57-62. [Crossref] [PubMed]
- Good medical practice 2014. Available online: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice
- Majid N, Lee S, Plummer V. The effectiveness of orthopedic patient education in improving patient outcomes: a systematic review protocol. JBI Database System Rev Implement Rep 2015;13:122-33. [Crossref] [PubMed]
- O'Connor MI, Brennan K, Kazmerchak S, et al. YouTube Videos to Create a "Virtual Hospital Experience" for Hip and Knee Replacement Patients to Decrease Preoperative Anxiety: A Randomized Trial. Interact J Med Res 2016;5:e10 [Crossref] [PubMed]
- McIntosh B, Cookson G, Jones S. Cancelled Surgeries and Payment by Results in the English National Health Service. J Health Serv Res Policy 2012;17:79-86. [Crossref] [PubMed]
- Ferguson C, Shandall A, Griffith G. Out-of-hours workload of junior and senior house surgeons in a district general hospital. Ann R Coll Surg Engl 1994;76:53-6. [PubMed]
- Ghiyasvandian S, Zakerimoghadam M, Peyravi H. Nurse as a Facilitator to Professional Communication: A Qualitative Study. Glob J Health Sci 2014;7:294-303. [Crossref] [PubMed]
- Nagpal K, Vats A, Lamb B, et al. Information transfer and communication in surgery: a systematic review. Ann Surg 2010;252:225-39. [Crossref] [PubMed]
- Choudhary A, Gupta V. Teaching communications skills to medical students: Introducing the fine art of medical practice. Int J Appl Basic Med Res 2015;5:S41-4. [Crossref] [PubMed]
- Goddard AF, Hodgson H, Newbery N. Impact of EWTD on patient: doctor ratios and working practices for junior doctors in England and Wales 2009. Clin Med (Lond) 2010;10:330-5. [Crossref] [PubMed]
- UK has fewer doctors per person than most other OECD countries. BMJ Careers. 2017. Available online: http://careers.bmj.com/careers/advice/UK_has_fewer_doctors_per_person_than_most_other_OECD_countries
- Wilson S, Jain N, Johnson D. Is the number of new trauma and orthopaedic consultant posts increasing or decreasing? Ann R Coll Surg Engl 2017;99:591-3. [Crossref] [PubMed]
- Cancelled Elective Operations. England.nhs.uk. 2018. Available online: https://www.england.nhs.uk/statistics/statistical-work-areas/cancelled-elective-operations/
- Ashton F, Hamid K, Sulieman S, et al. Factors Influencing patient experience and satisfaction following surgical management of ankle fractures. Injury 2017;48:960-5. [Crossref] [PubMed]
- Parsons BA, Blencowe NS, Hollowood AD, et al. Surgical Training: The Impact of Changes in Curriculum and Experience. J Surg Educ 2011;68:44-51. [Crossref] [PubMed]
- Best C, Wolstenholme S, Kimble J, et al. How ‘nil by mouth’ instructions impact on patient behaviour. Nurs Times 2004;100:32-4. [PubMed]
- Mehta SS, Bryson DJ, Mangwani J, et al. Communication after cancellations in orthopaedics: The patient perspective. World J Orthop 2014;5:45-50. [Crossref] [PubMed]
Cite this article as: Wasim AS, Shahban S, Goswami V. Hospital policy following cancelled orthopaedic surgery and the patient experience—making the best of a bad situation. J Hosp Manag Health Policy 2018;2:48.