Understanding the dynamics of non-clinical staff reallocation to clinical practice during the first wave of COVID-19—a qualitative study
Introduction
As the coronavirus disease 2019 (COVID-19) pandemic escalated worldwide in 2020, hospitals quickly had to take measures to prevent staff shortages. Not only could the pandemic result in an increased demand for patient care, but also a decrease in capacity due to clinical staff being infected (1-3). A successful staff contingency plan is pivotal to prevent the health care system from collapsing during a crisis such as the COVID-19 pandemic (4). In order to ensure capacity to deliver treatment and care for patients, one responsive strategy is reallocation of staff between departments. This strategy was implemented in various forms by many hospitals all over the world during the pandemic (5).
Previous research has studied barriers to reallocation and identified features of successful staff reallocation plans (2,3,5-8). Especially, staff’s ability and willingness to work have been perceived as important determinants of working behavior during a pandemic (2,6). Strategies to successful staff reallocation include continued tailored training programmes that meet staff’s individual learning needs and securing of a psychologically and physically safe work environment (3,5,9-11). Furthermore, previous research underlines the importance of well-defined communication channels to facilitate decision making (3,5,7), strategies to maximize the use of pre-existing skills (5,8), and a decentralized leadership approach (3,5).
Although a staff reallocation plan seems possible and sensible in theory, it may work differently when put into practice. During the COVID-19 pandemic, development and implementation of staff contingency plans had to happen fast under rapidly changing circumstances. In order to improve the implementation of future staff contingency plans it is important to understand how unpredicted situation-related moderating factors may influence implementation of a reallocation strategy under such conditions.
On March 11 2020, the World Health Organization (WHO) declared COVID-19 a pandemic (12), and the same day the Danish government closed down the country and changed COVID-19 strategy. Before, COVID-19 patients had been referred to six specialized hospitals, but from March 11 patients could be referred to all acute hospitals in the country (13). To ensure staff capacity, elective treatments, ambulatory care, and research were downscaled to release staff to acute care. At Bispebjerg & Frederiksberg Hospital in the Capital Region of Denmark, a staff contingency plan was formulated and implemented within one week. A part of the staff contingency plan included reallocation of staff from departments with low or non-clinical activities to clinical practice. At hospital level, without having an overview of the exact number, there was an expectation that it would be possible to reallocate numerous non-clinical staff. However, it quickly became apparent that fewer staff than expected were reallocated during the first wave of the COVID-19 pandemic. In this study we explore what influenced implementation of the hospital staff contingency plan that included reallocation of non-clinical staff during the first wave of COVID-19. We present the following article in accordance with the COREQ reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-14/rc).
Aim
The aim of the study is to explore the dynamics of reallocating non-clinical staff during a health care crisis in order to strengthen future implementation strategies and hence, reduce the gap between reallocation as planned and reallocation as done.
The research questions guiding the study were: How did leaders and staff experience the reallocation process during the first wave of COVID-19 and what affected how the contingency plan was put into practice?
Methods
Setting
Our study took place at Bispebjerg & Frederiksberg Hospital, a public 530-bed university hospital in the Capital Region of Denmark. The hospital is one of four acute hospitals in Copenhagen, and serves as a community hospital for around 450,000 citizens of the inner city and provides special services for an even larger population. The hospital attends to 80,000 acute and elective patients and has more than 400,000 outpatient visits per year. Medical specialties include: emergency medicine, intensive care, pulmonology, endocrinology, cardiology, gastroenterology and gastrointestinal surgery, geriatrics, neurology, dermatology, orthopedic surgery, occupational and environmental medicine, and social medicine. Additionally, the hospital includes several transversal specialties such as clinical pharmacology, biomedicine, radiology, physio- and occupational therapy, and a nurse floating pool. Furthermore, the hospital houses various research centers. Around 3,000 staff are permanently employed, of which 600 are doctors, around 1,240 are nurses, and 77 are nursing assistants.
Staff contingency plan
In March 2020 during the first wave of the COVID-19 pandemic, the hospital made several organizational changes to accommodate a surge of infected patients. A test center for patients who were referred to medical evaluation or test due to suspicion of COVID-19 was established. The test center was managed by the Emergency Department and staff consisted of the regular emergency staff, reallocated non-clinical staff, and medical students. The test center was open to self-referrals, patients referred from their general practitioner, or the regional central visitation. Patients with severe symptoms and a positive test were admitted directly from the test center. Patients brought to the hospital by ambulance were isolated and tested in a specific bed section in the emergency department before released to other units in the hospital.
Patients with a primary diagnosis of COVID-19 were admitted to the Emergency Department, Department of Pulmonary Medicine, or in severe cases the Intensive Care Unit. Furthermore, a new emergency bed unit was established for patients with a secondary COVID-19 diagnosis. The bed unit was staffed by reallocated staff from closed outpatient clinics, surgical departments, and reallocated non-clinical staff.
Staff from departments with low or non-clinical activities were reallocated to a staff floating pool, managed by the hospital’s nurse floating pool. The staff were mainly doctors working in research or specialized in occupational or social medicine, physiotherapists, pharmacists, or staff working in paraclinical departments.
Staff with recent clinical experience were assigned to clinical functions corresponding to a newly educated doctor or nurse. They were mainly reallocated to the newly established bed unit for COVID-19 patients, or the COVID-19 test center. Staff with little or no medical experience were assigned a new function as ‘Runner’, ‘Cleaner’, ‘Foodie’ or ‘Mixer’, which were functions created for the COVID-19 situation. Runners provided staff with the necessary equipment in the patient rooms, enabling the staff to stay with the patients and to economize the use of personal protective equipment (PPE). Cleaners continuously cleaned exposed areas to decrease the spread of infection, and foodies served meals to the patients. Mixers were in charge of dispensing medicine. These services aimed to release the regular staff and provide time for patient care. The staff were reallocated based on demand from all units handling COVID-19 patients. Consequently, the unit they were reallocated to could differ from day to day.
The board of directors asked all departments with low or non-clinical activities to identify staff that could be reallocated to the staff floating pool and perform the new job functions. To prepare the reallocated staff for their new tasks they participated in a mandatory 1-day course to learn about COVID-19, the hospital’s staff contingency plan, and to refresh basic clinical skills, as well as how to use PPE.
Design
The study design consisted of three parts; (I) A survey that was distributed to all non-clinical staff participating in the 1-day preparation course, (II) interviews with staff who were reallocated to the hospital’s floating pool as part of the staff contingency plan, and (III) interviews with leaders of the departments that contributed with staff for reallocation. This paper primarily describes the qualitative part of the study. We chose a qualitative approach as it could provide more in-depth knowledge and help us explore meanings and experiences influencing the dynamics of reallocation (6,14).
Framework
Brinkerhoff’s ‘Success Case Method’ (SCM) was chosen as a framework for the study. SCM was originally developed for evaluating the business effect of educational programs (15). According to Brinkerhoff, it is important to identify what works and what doesn’t, in order to improve a given effort (16). Furthermore, Brinkerhoff’s method is interesting as it is concerned with the knowledge you can obtain from studying the extremes instead of the mean. SCM operates with the terms ‘successes’ and ‘non-successes’, which is defined as the individuals who have been most and least successful in using new capabilities and methods (16). SCM consists of two steps: (I) a survey which aims at identifying potential successes and non-successes, (II) individual semi-structured interviews with selected successes and non-success, aiming at exploring which initiatives contributed to or hindered success (15). SCM has previously been applied in evaluating educational interventions in the health sector (17-19). In this study we used SCM to select the informants and design the interview guide for the reallocated staff.
Survey
The reallocated staff who participated in the hospital’s mandatory 1-day preparation course received an online survey one month after the course. We chose this timeframe to increase the possibility that the participants had taken shifts in clinical practice, but at the same time still were able to recall the details of the experience. A total of 174 hospital workers participated in the 1-day course, and 103 (59%) completed the online survey. Of those who completed the survey, 71 were employed at a department with low activity due to COVID-19 and participated in the hospital floating pool. A total of 55% of the staff were doctors, 13% were pharmacists, 8% were physiotherapist, 7% were nurses, and 4% were bioanalysts. Within the preceding month after participating in the 1-day course, 42 (59%) had one or more shifts in a clinical department. The number of shifts per worker ranged from 0 to 20, with a median of 2. A total of 36% of the respondents replied that they had not had patient contact within the last 3 years. Fourteen percent of the respondents replied that it had been more than 4 years since they had clinical experience and 11% had never occupied a position that included contact with patients.
One of the purposes of the survey was to help the researchers identify and purposefully select the eligible informants for the study. We selected the staff based on their reply to the question: “Overall, how would you rate your experience with handling a different function than usual?”. The staff were asked to reply on a scale from 1 to 6, with ‘1’ meaning “very poor” and ‘6’ meaning “very good”. According to the replies, five respondents (11%) had a poor or very poor experience (response category 1 or 2), whereas 11 respondents (18%) had a very good experience (response category 6).
In accordance with Brinkerhoff’s SCM (15), we selected eligible informants with replies indicating the most successful experience with being reallocated to clinical practice and the staff indicating the most unsuccessful experience. In order to obtain a wide variety in our material, the informants were also selected based on their assigned new function and their usual job function. Consequently, we invited ten members of the staff by e-mail to participate in the interview study.
Interviews with reallocated staff
We conducted individual semi-structured interviews (20) with selected reallocated staff. In line with Brinkerhoff’s SCM (15,16), we developed two separate interview guides: one for the staff with a successful experience (successes) and one for the staff with an unsuccessful experience (non-successes). Both interview guides were developed and refined by the research team. Brinkerhoff suggests that interviews with successes are based on five questions: (I) What did they use that worked? (II) What results were achieved? (III) What good did it do (value)? (IV) What helped? and (V) Suggestions. Interviews with non-successes should be based on questions related to: (I) barriers and (II) suggestions (16). Consequently, the interview guide for the staff with the most successful experience included: (I) which factors contributed to the reallocation being a positive experience, (II) their own experienced contribution, (III) what made them feel safe in their new function, and (IV) barriers, if any, in relation to managing the new function. The interview guide for the staff with an unsuccessful experience included: (I) what went wrong, (II) contributing factors for the unsuccessful experience, and (III) barriers for managing the new function. Both groups were asked for improvement suggestions.
The informants chose the setting for the interviews. Therefore, some interviews were conducted at the informants’ department, whereas others took place in the researchers’ department or online. Two members of the research team (RLR Johansen and C Emme) conducted the interviews. During all interviews, one of the two members observed the interview and took field notes. All interviews were audio-recorded. However, full transcription was not conducted due to limited resources. Instead, selective transcription was performed by the same two members of the research team, picking out relevant passages, in terms of answering the research questions, and noting the tape counter numbers to mark quotations (21).
Interviews with leaders
By e-mail we invited leaders of all eight departments which reallocated staff to participate in the study. The interviews were semi-structured and based on an interview guide, developed by and discussed in the research team. The interview guide consisted of four main questions together with supporting questions concerning the leaders’ reflections on reallocating their staff to clinical practice and handling COVID-19 related tasks. The leaders chose the setting for the interviews. Most interviews were conducted at the leader’s office, and one was performed online.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). According to Danish law, only biomedical research requires permission from the Regional Scientific Ethical Committee (22,23). Furthermore, the research group requested permission from the Danish Data Protection Agency, but this was not required.
The informants received an e-mail invitation with information about the study. Before the interview they also received oral information and signed a consent form. In order to respect the informants’ anonymity, we replaced their names with codes in the data (e.g., S1). Leaders were coded as L1–L8.
Analysis
Data was analyzed using inductive content analysis, which enables obtaining results based on the participants’ perspectives without imposing preconceived categories (24,25). We used researcher triangulation to strengthen the credibility of the results (26). Consequently, data was analyzed by two researchers with different educational backgrounds (public health science and nursing science) and discussed with the rest of the research group, providing more perspectives to the analysis (24,27). The researchers initiated the analysis by listening to the recordings of the first interview together, making sense of the data, and then performed open coding. The initial codes were discussed and elaborated on, with the initial grouping of the data. Next, the researchers listened to and coded the remaining interviews separately, and subsequently the researchers discussed and merged their codes, resulting in joint categorization and abstraction. Disagreement was solved through dialogue. An example of the analysis process is illustrated in the coding tree (see Table 1). Data saturation, results, and abstraction were discussed with the research team in order to ensure rigour and minimize analysis bias (28). All data was managed in Microsoft Word.
Table 1
| Data | Code | Subcategory | Category |
|---|---|---|---|
| “It also made me feel confident that there was always a doctor in the ward with whom you could discuss the patients. I felt that everybody was very forthcoming. Sometimes the medical specialists also asked me for advice. And sometimes I asked them. There was a constant exchange of information” | Always somebody to ask | Collegial sparring | Psychological factors |
| “I have always felt supported when I was in these departments. And you can always ask. I´m not afraid of asking” | Not being afraid to ask questions |
Results
Between May 28 and July 6, 2020, we conducted 14 interviews with eight leaders and six staff members. Leaders from seven of the eight departments participated and the last did not respond to the invitation. One department had shared leadership, and consequently we interviewed both leaders together. Six out of ten invited staff participated in the study; three did not respond to the invitation and one cancelled at the last minute. The interviews with both leaders and staff had a mean duration of 21 minutes (range, 17–31 for leaders and range, 18–27 minutes for staff). For further information about the staff see Table 2.
Table 2
| ID | Age (years) | Usual job function | Years since participating in clinical practice | Assigned new function | No. of shifts in clinical departments |
Success/ non-success |
|---|---|---|---|---|---|---|
| S1 | 34 | Physician | Still in clinical practice | Doctor in Corona Test Center | 5 | Success |
| S2 | 61 | Physiotherapist | Still in clinical practice | Cleaner/foodie/runner | 15 | Success |
| S3 | 63 | Physician | >5 | Doctor in Corona Test Center | 3 | Non-success |
| S4 | 30 | Physician/researcher | <1 | Clinical doctor corresponding to a newly educated doctor | 5 | Success |
| S5 | 35 | Physician/researcher | <1 | Doctor in Corona Test Center | 2 | Non-success |
| S6 | 57 | Master of Science (MSc) | Never in clinical practice | Runner | 4 | Success |
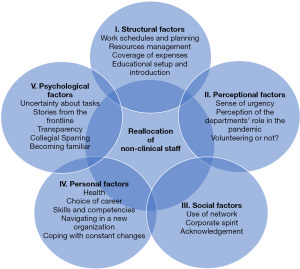
We identified several moderating factors related to the dynamics of reallocating staff from departments with reduced activities to the COVID-19 test center or bed units during the first wave of the pandemic. We categorized the factors as: (I) structural, (II) perceptional, (III) social, (IV) personal, and (V) psychological. Figure 1 provides an overview of the five categories and subcategories.
Structural factors
Identified moderating factors were categorized as structural factors if they were related to the contingency plan set-up. One structural challenge was work schedules and planning. When staff were needed to cover a shift, a text message offering the shift was sent to all staff reallocated to the floating pool, which they could accept or decline. The first person to accept the shift received a confirmation, and the rest did not get further information. Some informants perceived this procedure as flexible, whereas others found it difficult to plan ahead and lacked a general view of which shifts had already been taken. In addition, the flexibility of the staff was challenged by schools and childcare institutions being closed during the first wave of the pandemic.
“The text message worked well. Or in general it worked well. Sometimes you were offered 10, maybe 15 different shifts, and even though you replied quickly, you might not get the three shifts you wanted and were left with shifts that did not match with your family or other tasks […] It would have been nice with more transparency.” (S1, success, physician, Corona Test Center).
Not all staff had been properly informed about the registration procedure. Several informants had expected a fixed work schedule or expected to be reallocated to only one department. The uncertainty about the registration procedure led some staff to seek out shifts themselves, bypassing the floating pool agency. Furthermore, it could be difficult for the staff to know to what extent they should prioritize the shift over their usual tasks, and some were insecure about how many shifts they were expected to cover.
A second structural factor was resource management. Although most of the staff were sent home due to the COVID-19 restrictions, they were not necessarily available for reallocation. The departments needed staff to secure day-to-day operations, and some departments had tasks directly related to handling COVID-19, which required retainment of staff.
“Suddenly we had a lot to do, and I couldn’t just say that everybody could cover [COVID-19] shifts. So I retained staff.” (L1).
Thus, what in theory looked like staff that could be reallocated, was not in practice.
How the pandemic influenced usual tasks affected the staff’s experience with being reallocated. Some staff could easily work remote, and to them the clinical shifts were perceived as an add-on, clashing with their everyday and family life.
“To me it was all about, how does it affect my everyday life? How does it affect my family and my usual work? It was extra work. It was hard to fit my schedule.” (S5, non-success, physician, Corona Test Center).
Furthermore, the staff contingency plan did not outline the order in which staff should be prioritized for reallocation, and often the text message with an available shift was sent out to a large group of staff without consideration of prioritization. The lack of order of priority affected some of the staff negatively, as they believed that there should have been a more systematic approach, like initially reallocating the staff unable to work remote. In addition, shifts were offered to the staff directly, without involving their leaders. This feature made it difficult for the leaders to form a general overview of which staff were available for other tasks and prioritize who should be reallocated, leading to a feeling of poor resource utilization among both leaders and staff. Another contributing factor to the feeling of poor resource usage was the experience by some of the staff of having nothing to do on their shifts, which frustrated them. Also, some leaders experienced having spare staff but no demand from the clinical units, which surprised the leaders as they knew that some departments were overloaded. This also added to the feeling of poor resource utilization.
A third structural factor influencing the reallocation process was the coverage of expenses. The departments were expected to cover the salary expenses of their staff during their reallocation, as shifts were meant to replace ordinary work and not to be extra work. The reallocated staff usually only worked daytime, but often the COVID-19 shifts were evening- or night-shifts. The expenses became a big concern for some leaders as the departments had not budgeted with shift allowances.
“It became much more expensive than necessary. A lot of staff were sent home. But we had no control over which staff were offered and accepted a shift. It was unclear whether it was ‘nice to’ or ‘need to’. It became like pick n mix sweets, without my involvement. It didn’t make sense, financially.” (L1).
As a result, some of the staff experienced restrictions on which shift they could cover, and thereby not being able to contribute to the extent that they wanted. Coverage of expenses was also a challenge for staff whose salary was covered by funds, such as PhD students, as the departments had to cover all expenses for this type of employees.
The final identified structural factor was educational setup and introduction. As preparation to reallocation, the staff participated in a 1-day course, providing theoretical knowledge, a brush-up on clinical skills and brief introduction to COVID-19 related tasks. In general, the staff preferred hands-on exercise rather than theoretical training, for example practicing application of peripheral venous catheters. When possible, the staff were offered a tour in the COVID-19 test center. The actual introduction to new tasks was performed in the units. How the staff were introduced to the unit they were reallocated to varied. Some of the reallocated staff experienced a very organized and detailed introduction to the unit. Others experienced that the regular staff did not know they were coming, or a lack of instruction, resulting in the staff defining their own tasks.
Perceptional factors
Some of the factors that modified how staff were reallocated were related to how staff and leaders interpreted the staff contingency plan in the context of their own understanding. These factors were categorized as perceptional factors.
The perception of sense of urgency by both staff and leaders, influenced their motivation and behavior related to reallocation, in particular in the beginning of the first wave of the pandemic. The situation in other parts of the world portrayed in the media formed the burning platform. However, as the first wave of the COVID-19 pandemic evolved, the sense of urgency changed. The pandemic seemed to be under control, and consequently the burning platform became less apparent, which led staff and leaders to prioritize usual tasks.
Another perceptional factor was the leaders’ perception of the departments’ role in the pandemic, as their understanding influenced their expectations to the involvement of their staff. All leaders were ready to contribute with staff, but many leaders did not think of their department as the first choice, as they perceived the department to differ from other departments.
“We are part of the hospital, but we are different… we are not the ones who stand first in line.” (L8).
Finally, the question of volunteering or not was an important perceptional factor, which may have had great influence on the reallocation process. It was unclear to the leaders whether participation was voluntary or not, and this affected how they framed reallocation to their staff. Several leaders framed reallocation as voluntary, especially if they did not perceive their staff as the obvious first choice. For these leaders the staff’s motivation for being reallocated was important. Other leaders perceived their staff to be first in line. They framed participation as a duty and expressed to their staff that reallocation was mandatory. Some of the leaders experienced dilemmas concerning reallocation of their staff. For some it had not been an easy choice whether reallocation should be voluntary or not. Also, the leaders were concerned about how their staff would react to being reallocated, and how the decision would affect their professional relation.
“It was difficult as a leader. Should I force them to reallocate? It would probably have had some consequences.” (L8).
The reallocated staff had diverse experiences concerning whether they had felt pressured to reallocate. Some had experienced the reallocation as completely voluntary, whereas others had felt an expectation or pressure from their leader or the hospital management.
“We were told that we wouldn’t be forced, but we were encouraged”. (S6, success, MSc, runner).
Social factors
The process of reallocation was also perceived by the leaders and staff in a social context. One identified social factor was the use of network. The relationship to the hospital management and the management of the floating pool agency influenced how the leaders overcame the challenges with shift planning and lack of transparency in structural factors. Some leaders used their network and made individual agreements about reallocation of staff, which resulted in a better balance between the demand for reallocation and the need for staff to secure day-to-day operations in the department.
Another social factor was corporate spirit, as it was important to the leaders to demonstrate ‘esprit de corps’ by actively participating in the crisis management. The leaders all felt an obligation and motivation to contribute as they felt a sense of cohesion with the rest of the hospital. The feeling of cohesion and sense of urgency promoted a proactive behavior among the leaders. For example, some leaders expressed a willingness to be reallocated themselves. Furthermore, several leaders independently offered their contribution before the staff contingency plan was developed.
“I had already told the CEOs of the hospital that we had many available physicians. We were ready to contribute. I had already told my staff that they should expect changes, and that their work tasks could change radically.” (L7).
Finally, acknowledgement was a social factor influencing the reallocation process. The staff who had a positive experience with being reallocated felt that their contribution made a difference and was appreciated by the clinical staff. Several of the reallocated staff received positive comments, which added to the feeling of being needed.
“What made it a positive experience was the feeling of doing something important for other people. When I was in the Corona Test Center, I was in contact with many different people, and I often got comments like: ‘Good Job’. That made me feel good.” (S6, success, MSc, runner).
Personal factors
Whether staff were successfully reallocated was influenced by personal factors, such as health, skills, and personal characteristics.
The health of the employees was an important personal factor affecting the leaders’ choice of which staff could be reallocated. Consequently, staff were not reallocated if they had any health issues. The leaders did not have any predefined criteria, but typically staff with chronic diseases, pregnancy, older staff, and staff who were concerned for their own health were excepted from reallocation.
Another personal factor influencing reallocation was the leaders’ consideration of the employees’ choice of career. For a large group of the staff it had been many years since they had worked in the clinical setting. Many of them had deliberately chosen a career that did not involve any clinical work.
“For some being in clinical practice led to anxiety. Some choose our specialty because they don’t want a life as a doctor.” (L7).
This was a consideration that the leaders had to take into account when selecting who to enroll for reallocation. It was not always an easy decision for the leaders to protect one employee and at the same time asking others to work at the front line.
“I was a bit concerned about how to tell the junior doctors that the senior doctors could stay at home and relax while they had to be sent into the lion’s den. However, it was never an issue for the junior doctors.” (L4).
Skills and competencies were also personal factors which affected the non-clinical staff’s decision to be reallocated. Being away from clinical practice for several years made some of the staff question whether they still had the skills to perform certain tasks. This made the staff consider what kind of functions they would feel comfortable being assigned to.
“For me a great barrier was fear. Am I skilled enough to do this?” (S5, non-success, physician, Corona Test Center)
The staff’s ability to navigate in a new organization was also a personal factor contributing to the staff’s experience with the reallocation process. Prior knowledge of the department or unit made the staff feel more comfortable and made it less difficult to re-enter clinical practice. Staff without previous knowledge of the unit had to spend time and energy to figure out the workflows and use of local professional language. It was not always easy to ask the permanent staff for help when things were busy, and often abbreviations were used which made no sense to the reallocated staff.
In addition, how staff coped with the constant changes was a personal factor. A great part of the non-clinical staff was reallocated to the newly established COVID-19 test center, which was continuously developed during the first wave. The staff described shifts in the test center as being chaotic in the beginning. They experienced a lack of leadership and information. Roles were undefined and nobody assigned tasks to the staff. The staff had to deal with constant changes as workflows, guidelines, and the national test strategy continuously changed. How the reallocated staff experienced the dynamic environment varied. For some it led to frustration or insecurity, others were unaffected, which was also pointed out by the leaders:
“Some people are able to contain uncertainty very well, and others need clear arrangements. […] For the staff who need clear arrangements, it was a difficult period. And then you have the kind of people who just say ‘well, that sounds exciting’.” (L7).
Consequently, how staff coped with the constant changes and lack of structure may have influenced their willingness to reallocate and to cover shifts.
Psychological factors
Moderating factors were categorized as psychological factors if they resulted in an emotional response.
Psychological safety was a recurring theme throughout the interviews with both staff and leaders.
A psychological factor was uncertainty about tasks. The uncertainty about what was expected of the staff made some feel insecure about being reallocated. Sometimes the staff were unsure of the professional standards, and in certain situations some staff expressed concerns about whether they could perform their tasks properly, e.g., assisting with sampling of tests. Despite insecurity about the tasks, the staff with an overall good experience emphasized that they felt less insecure when colleagues were forthcoming, introduced them to the tasks, and corrected potential errors. If the staff knew what to expect, they seemed to feel less insecure about being reallocated.
Another psychological factor was stories from the frontline which affected some of the staff. Rumours of cardiac arrest and critically ill patients made some staff worried about what could happen on a shift, which added to the feeling of uncertainty and anticipatory anxiety.
Also, transparency was a psychological factor influencing the reallocation process. For some of the reallocated staff transparency and honesty were important contributors to accepting the uncertainty and having a positive experience with being reallocated.
“There were two chief physicians on call you could always ask. They were always honest; ‘I don’t know. I’ll get back to you.’ Transparency was nice. As long as you got an honest answer, you knew that you just had to buckle down.” (S1, success, physician, Corona Test Center).
The reallocated staff emphasized the importance of collegial sparring, which made them feel more confident in their new assignment. Several of the staff expressed that it was legitimate to ask questions, and that collegial sparring was always available.
“It also made me feel confident that there was always a doctor in the ward with whom you could discuss the patients. I felt that everybody was very forthcoming.” (S1, success, physician, Corona Test Center).
Finally, becoming familiar with a new unit and new tasks influenced the reallocation of staff. Feeling familiar with a unit increased the reallocated staff’s confidence in their skills and competencies. Consequently, some staff chose to primarily sign up for shifts in units they were familiar with. In addition, the staff expressed that a regular workplace was not only a personal advantage but also an advantage for the permanent staff on the ward, because they had to spend less time introducing new staff, providing more time to their core tasks. This feeling may have supported the staff in their choice of selecting shifts in familiar wards, and at the same time choosing not to take shifts in units they were unfamiliar with.
Discussion
During the first wave of the COVID-19 pandemic reallocation strategies had to be implemented under rapid changing circumstances. No one knew how the pandemic would evolve or how it would affect the health care system. In this study we combine a staff- and leadership perspective to better understand the gap between reallocation as expected and reallocation as done. Our findings emphasize how implementation of a staff contingency plan is influenced by a complex set of structural, perceptional, social, personal, and psychological moderating factors.
In our study we found that even though staff felt obligated and motivated to work and intended to cover shifts, reallocation was influenced by several other factors related to the contingency plan set-up, how the contingency plan and roles were interpreted by staff and leaders, and how the leaders prioritized tasks and staff time. Furthermore, the reallocated staff used a lot of energy when they tried to navigate the workflows and understand the local professional language. Previous research highlights reallocation into task based teams as a way to maximise use of existing skills and ensure clear delineation of the roles (3,8). In our study shift planning was a major theme for both leaders and staff. The procedure for on-duty scheduling influenced how the staff signed up for shifts and how human resources were utilized at hospital level. The lack of overview of which staff should be prioritized led to a feeling of poor resource utilization among both staff and leaders. In nine interviews with leaders from five different countries, Panda et al. similarly found a need to better manage staff resources by matching available staff with the demand from clinical practice (5). To strengthen future staff contingency plans and reduce waste of resources, the reallocation process should include a strategy to prioritize staff for reallocation based on the demand from clinical practice, available staff, competing tasks and individual skills (3,5,8).
In this study we also highlight the importance of understanding how staff and leaders make interpretations and adjustments to a given plan in a social context. We found that staff and leaders navigated the system and tried to adjust to the situation, for example when the leaders made individual arrangements with the management of the floating pool to sustain control of their staff. Also, as the sense of urgency declined, the leaders and staff adjusted to the situation. Some adjustments may benefit the overall shared goal of handling the crisis efficiently, whereas other adjustments may be counterproductive. Panda et al. argue for a decentralized leadership approach to reallocation where local leaders are empowered to define local implementation strategies (5). Our study supports the potential of a decentralized approach, but also highlights the importance of studying the local implementation strategies. How leaders and staff adjust to a given overall plan can only be studied when the plan is in action, and therefore future staff contingency plans should consider how to evaluate such dynamics real-time to be able to improve the plan. During the COVID-19 pandemic such an evaluation strategy was applied by Camilleri et al. to develop a training programme for reallocated staff. Through daily feedback sessions they adjusted the training programme according to constant changes and needs (29). Similar rapid cycles of iterations could be applied to the overall staff contingency plan. For future recommendation, Ovretveit et al. suggest to combine implementation and improvement science to enable faster and more effective implementation of changes in rapidly changing situations, such as the COVID-19 pandemic. For example, implementation strategies should consider models of contextual variables as barriers and facilitators of implementation and include rapid cycle testing to provide timely feedback on effects and needed adjustments (30).
Finally, this study adds to the growing body of literature focusing on the psychological stress and anxiety related to reallocation (7,10,11,31,32). A psychologically safe environment in which it is legitimate to ask questions, may reduce stress and increase the feeling of safety. Edmondson et al. define ‘psychological safety’ as people’s perception of the consequences of taking interpersonal risks in a particular context. A psychologically safe environment is characterized by staff not being afraid of asking questions or expressing concerns. Instead, staff seeks information exchange with others, which fosters a trusting relationship. Focus is on the collective goal rather than on self-protection (33). Similar to previous research (3), the reallocated staff in our study emphasized the importance of collegial sparring and transparency. They also highlighted a feeling of mutual respect and trusted that colleagues would speak up if they made a mistake. It is interesting how staff experienced insecurity about tasks, chaos, and lack of leadership, especially in the newly established test center, and at the same time expressed a high degree of psychological safety. In the Corona Test Center, everyone was new to the work, and no interpersonal hierarchy existed. This may have led to a shared understanding of the importance of mutual support. Also, the staff in our study may have felt less need to protect their own professional identity, as they did not usually work in a clinical setting and therefore may have felt that it was more legitimate to be open about their own limitations.
Strengths and limitations
One of the main strengths of this study is that it takes on a different perspective than many of the existing studies focusing on the frontline staff only. By focusing on the non-clinical staff and leadership perspectives we gain a better understanding of the barriers and promoters of the reallocation of staff, which may be important in future contingency plans.
One of the limitations of this study is that the interviews were not fully transcribed, which entails a risk of the researchers overlooking important aspects. To decrease this risk, the researchers worked closely together in the analysis process, in particular during the first phases; making sense of the data, open coding, and grouping (24).
Another important perspective is whether this reallocation was actually valuable to the clinical departments. Originally, we incorporated this perspective in the design of the study, but due to limited time we only succeeded in interviewing two leaders from departments receiving help from reallocated non-clinical staff. As data was limited, we chose not to include the results in this study. However, one of the important points was that it was considered time- and resource consuming to introduce the reallocated staff. Consequently, the leaders preferred to use their regular staff to cover the new functions, which may have contributed to the non-clinical staff not being reallocated to the expected extent during the first wave of the pandemic.
The staff interviews were inspired by Brinkerhoff’s SCM (15,16), which was applied in the sampling process and in the development of the interview guide. SCM helped us shed light on the factors contributing to the dynamics of reallocation of staff during the first wave of COVID-19. One of the advantages of the SCM is the focus on the respondents with the most positive and negative experiences to provide knowledge of the factors that contributed to a successful or non-successful reallocation experience. This helped us obtain a broad view of contributing factors, which may increase the trustworthiness and credibility of the study (34,35).
Both successes and non-successes reported promoters and barriers to reallocation, and consequently we were unable to identify factors that clearly differentiated the two groups. This may be due to the limited number of informants.
Implications
To strengthen future staff contingency plans and reduce waste of resources, the reallocation process should include a strategy to prioritize staff for reallocation based on the demand from clinical practice, available staff, competing tasks, and individual skills. Furthermore, it is important to understand how reallocated staff and leaders interpret and adjust to a given plan, as this may have great influence on how the contingency plan is put into practice. In addition, both researchers and managers of future staff contingency plans should consider how to evaluate such dynamics real-time to be able to improve the plan.
Conclusions
This study identified a variety of complex moderating factors, which should be considered when hospital staff contingency plans are implemented. The study highlights the importance of understanding how reallocated staff and leaders experience and make interpretations and adjustments to a given plan, as this may have great significance for how the contingency plan is put into practice. Future staff contingency plans should take these factors into consideration to make better use of human resources in times of crisis and to improve staff’s experience with reallocation.
Acknowledgments
The authors would like to thank the staff and leaders participating in this study. Furthermore, we would like to thank Bjørn Hesselbo, Senior Consultant, for his assistance with setting-up and distributing the survey to the participants.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the COREQ reporting checklist. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-14/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-14/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-14/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-14/coif). MSL reports having received research funding for his department from Merck Sharp & Dohme for research outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from all informants. According to Danish law, only biomedical research requires permission from the Regional Scientific Ethical Committee. Furthermore, the research group requested permission from the Danish Data Protection Agency, but this was not required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. COVID-19 strategy update [Internet]. 2020. Available online: https://www.who.int/publications/m/item/covid-19-strategy-update
- Aoyagi Y, Beck CR, Dingwall R, Nguyen-Van-Tam JS. Healthcare workers' willingness to work during an influenza pandemic: a systematic review and meta-analysis. Influenza Other Respir Viruses 2015;9:120-30. [Crossref] [PubMed]
- Vera San Juan N, Clark SE, Camilleri M, et al. Training and redeployment of healthcare workers to intensive care units (ICUs) during the COVID-19 pandemic: a systematic review. BMJ Open 2022;12:e050038. [Crossref] [PubMed]
- World Health Organization. COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 March 2020 [Internet]. 2020. Available online: https://apps.who.int/iris/handle/10665/331561
- Panda N, Sinyard RD, Henrich N, et al. Redeployment of Health Care Workers in the COVID-19 Pandemic: A Qualitative Study of Health System Leaders' Strategies. J Patient Saf 2021;17:256-63. [Crossref] [PubMed]
- Lee HJ, Kim E, Morse BL, et al. Barriers and Facilitators of Nurses' and Physicians' Willingness to Work during a Respiratory Disease Outbreak: A Mixed-Methods Systematic Review. Int J Environ Res Public Health 2021;18:6841. [Crossref] [PubMed]
- Walker KL, Gerakios F. Redeployment during the first wave of the COVID-19 pandemic: implications for a clinical research workforce. Br J Nurs 2021;30:734-41. [Crossref] [PubMed]
- Doyle J, Smith EM, Gough CJ, et al. Mobilising a workforce to combat COVID-19: An account, reflections, and lessons learned. J Intensive Care Soc 2022;23:177-82. [Crossref] [PubMed]
- Danielis M, Peressoni L, Piani T, et al. Nurses' experiences of being recruited and transferred to a new sub-intensive care unit devoted to COVID-19 patients. J Nurs Manag 2021;29:1149-58. [Crossref] [PubMed]
- Khajuria A, Tomaszewski W, Liu Z, et al. Workplace factors associated with mental health of healthcare workers during the COVID-19 pandemic: an international cross-sectional study. BMC Health Serv Res 2021;21:262. [Crossref] [PubMed]
- Coughlan C, Nafde C, Khodatars S, et al. COVID-19: lessons for junior doctors redeployed to critical care. Postgrad Med J 2021;97:188-91. [Crossref] [PubMed]
- World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- The Prime Minister’s Office. Press meeting about COVID-19 March 11th 2020 [Internet]. Available online: https://www.stm.dk/presse/pressemoedearkiv/pressemoede-om-covid-19-den-11-marts-2020/
- Miller W, Crabtree B. Clinical research. A multimethod typology and qualitative roadmap. In: Crabtree B & Miller W (editors). Doing qualitative research. 2nd edition. Thousand Oaks: SAGE Publications, 1999:3-30.
- Brinkerhoff RO. The Success Case Method: A Strategic Evaluation Approach to Increasing the Value and Effect of Training. Advances in Developing Human Resources 2005;7:86-101.
- Brinkerhoff RO. The Success Case Method. Find out quickly what’s working and what’s not. San Francisco: Berrett-Koehler Publishers, 2003.
- Eid A, Quinn D. Factors predicting training transfer in health professionals participating in quality improvement educational interventions. BMC Med Educ 2017;17:26. [Crossref] [PubMed]
- Olson CA, Shershneva MB, Brownstein MH. Peering inside the clock: using success case method to determine how and why practice-based educational interventions succeed. J Contin Educ Health Prof 2011;31:S50-9. [Crossref] [PubMed]
- Shershneva MB, Larrison C, Robertson S, et al. Evaluation of a collaborative program on smoking cessation: translating outcomes framework into practice. J Contin Educ Health Prof 2011;31:S28-36. [Crossref] [PubMed]
- Kvale S, Brinkmann S. Interviews. Learning the craft of qualitative research interviewing. 2nd edition. SAGE Publications, 2009.
- Robson C, McCartan K. Interviews and focus groups. In: Real world research - A resource for users of social research methods in applied settings. 4th edition. Wiley 2016:284-306.
- Official Danish online legal portal covering legislation etc. from government departments. Act on scientific ethic processing of health sciences research projects [Internet]. 2011. Available online: https://www.retsinformation.dk/eli/lta/2011/593
- National Comitee on Health Research Ethics. Act on Research Ethics Review of Health Research Projects [Internet]. Available online: https://en.nvk.dk/rules-and-guidelines/act-on-research-ethics-review-of-health-research-projects
- Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107-15. [Crossref] [PubMed]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277-88. [Crossref] [PubMed]
- Carter N, Bryant-Lukosius D, DiCenso A, et al. The use of triangulation in qualitative research. Oncol Nurs Forum 2014;41:545-7. [Crossref] [PubMed]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004;24:105-12. [Crossref] [PubMed]
- Smith J, Noble H. Bias in research. Evid Based Nurs 2014;17:100-1. [Crossref] [PubMed]
- Camilleri M, Zhang X, Norris M, et al. Covid-19 ICU remote-learning course (CIRLC): Rapid ICU remote training for frontline health professionals during the COVID-19 pandemic in the UK. J Intensive Care Soc 2022;23:183-90. [Crossref] [PubMed]
- Ovretveit J, Mittman BS, Rubenstein LV, et al. Combining Improvement and Implementation Sciences and Practices for the Post COVID-19 Era. J Gen Intern Med 2021;36:3503-10. [Crossref] [PubMed]
- Lim C, De Silva I, Moussa G, et al. Redeployment of ophthalmologists in the United Kingdom during the Coronavirus Disease Pandemic. Eur J Ophthalmol 2021;31:2268-74. [Crossref] [PubMed]
- Martinez M, Stewart NH, Koza AL, et al. The Effect of Redeployment During the COVID-19 Pandemic on Development of Anxiety, Depression, and Insomnia in Healthcare Workers. J Gen Intern Med 2022;37:1003-5. [Crossref] [PubMed]
- Edmondson A. Psychological safety and learning behavior in work teams. Administrative Science Quarterly 1999;44:350-83.
- Elo S, Kääriäinen M, Kanste O, et al. Qualitative Content Analysis: A Focus on Trustworthiness. SAGE Open 2014; [Crossref]
- Morse JM, Barrett M, Mayan M, et al. Verification Strategies for Establishing Reliability and Validity in Qualitative Research. Int J Qual Methods 2002;1:13-22.
Cite this article as: Johansen RLR, Sørensen A, Langelo MS, Mikkelsen KH, Emme C. Understanding the dynamics of non-clinical staff reallocation to clinical practice during the first wave of COVID-19—a qualitative study. J Hosp Manag Health Policy 2022;6:32.