
A paramedic patient flow coordinator improves ambulance offload times in the emergency department
Introduction
Over 136 million patients visit emergency departments (ED) in the United States each year (1). Approximately 20 million of these patients arrive by ambulance (2). EDs across the country struggle with overcrowding, and the number of patients awaiting assessment, undergoing treatment, or awaiting discharge frequently exceeds ED resources (3). The problem of overcrowding is further compounded by increased ED utilization, a decrease in total number of inpatient beds, a decrease in the number of EDs, and a higher inpatient census (4).
One consequence of crowded and resource-depleted EDs is an increase in turnaround times for ambulance crews. Emergency medical services (EMS) turnaround time can be divided into off-load time, which is the time from hospital arrival to patient care turnover to the hospital staff, and recovery time, which is the time from patient turnover to hospital departure. Carter et al. found that off-load time accounts for approximately 70 percent of turnaround time (5). Prolonged off-load times can lead to delays in time to triage, time to physician, definitive patient care, and are an independent predictor of ED length of stay exceeding four hours (6). A 2006 Centers for Medicare and Medicaid Services statement warned that prolonging patient offload times may violate the Emergency Medical Treatment and Labor Act (EMTALA) and 42 CFR 482.55, the Conditions of Participation for Hospitals for Emergency Services (7). Furthermore, by forcing EMS crews to spend more time at hospitals, extended turnaround times decrease the number of available EMS crews available and place communities at risk of inadequate emergency services (7).
In order to decrease ambulance offload times, we implemented a paramedic patient flow coordinator (PPFC) in our ED. The PPFC is a full time staff member whose job is to assist the charge nurse and triage nurse in coordinating patient flow and bed assignments for patients arriving by air transport, ground EMS, and private vehicle. To determine whether the PPFC may assist in improving patient offload times, we compared offload time data from the 12 months immediately preceding our intervention to the 12 months immediately following implementation of the PPFC. To our knowledge, this is the first study investigating the benefit of a PPFC for patients arriving to the ED by ambulance. We present the following article in accordance with the SQUIRE reporting checklist (available at http://dx.doi.org/10.21037/jhmhp-20-26) (8).
Methods
We conducted a retrospective review of data before and after the implementation of the PPFC at a single academic tertiary care facility with an annual volume of 56,000 patients and an EMS catchment area of approximately 1.5 million people. Data on ED arrivals, EMS traffic, patient admission rates, and National Emergency Department Overcrowding Scores (NEDOCS) were compiled as part of ongoing, internal, departmental quality improvement measures. Because this study did not involve individual patients or review of patient data, it was not subject to review by the Institutional Review Board.
Starting July 1, 2017, we stationed the PPFC near the ambulance receiving doors in an area of maximal visibility in the department. The PPFC maintains constant communication with the triage nurse, charge nurse, and medical control for EMS by radio. In addition, the PPFC has computerized access to bed assignment information throughout the hospital, providing the most current information on patient departures from the ED and bed availability. On arrival, the PPFC does a limited reception of the patient into the computer and assigns the bed to which the patient is then offloaded. The nurse who will be caring for the patient then receives the EMS report, with completion of the full triage note at a later time.
Retrospective data were compiled into reports that had been derived from electronic medical record data at the department level for each month. Data was extracted using agency-specific software for EMS A and EMS B (made anonymous for this study as some EMS agencies in our community are commercial entities), which account for roughly 50% of all EMS traffic to the study site. In total, approximately 40 agencies contribute to EMS traffic at our facility. We do not have access to electronic data tracking for other EMS agencies, which precluded inclusion of data from those arrivals.
Data was collected from two separate twelve-month time periods: July 2016 to June 2017 and July 2017 to June 2018. Data included all patients who arrived at the ED by EMS A’s or EMS B’s ambulance services during the study period unless otherwise excluded. Data excluded pediatric patients (except in rare cases of trauma patients 15 years of age or older), pregnant patients over 20 weeks with non-traumatic related emergencies, patients who arrived by private vehicle, patients who arrived by other EMS agencies including air transport, and patients who arrived by ambulance but were triaged to the ED’s waiting area.
Data for the month immediately prior to and following the implementation of the PPFC was excluded to account for offload time variation during the implementation period. We also accounted for the implementation of a medical admissions unit (MAU) in March 2017. We compared offload time and ED crowding data for the three months immediately prior to (December 2016–February 2017) and after (April 2017–June 2017) the implementation of the MAU (Table 1). To determine whether these months might differ in EMS offload times or ED crowding measures at baseline, we utilized corresponding measures from the next calendar year as the control time period (December 2017–February 2018 and April 2018–June 2018). We found that the MAU opening correlated with a statistically significant decrease in offload time (30.87 versus 22.08 minutes, P=0.01) as well as an increase in the number of offload times less than 20 minutes (130.3 versus 300, P=0.04) and the percent of offload times less than 20 minutes for EMS A (25.8% versus 52.4%, P=0.02), but not EMS B (Table 1). The number of boarding hours for patients in the ED (11,070 versus 6,576, P=0.03), but not NEDOCS, also decreased after the opening of the MAU. We therefore accounted for the decrease in EMS A offload time, EMS A offloads less than 20 minutes (number and percent), and boarding hours in our statistical analysis. An appropriate proportion of these values was applied to March to account for the time following the implementation of the MAU. Data comparisons were conducted using Student’s t-tests with a Bonferroni-Dunn correction factor for multiple t-tests (adjusted P values). Data compilation and statistical analyses were performed using Microsoft Excel (Microsoft, Redmond, WA) and Graphpad Prism (San Diego, CA).
Table 1
| Variable | Medical admissions unit | Control time | ||||||
|---|---|---|---|---|---|---|---|---|
| 12/2016–2/2017 | 4/2017–6/2017 | Difference (SE) | Adjusted P value | 12/2017–2/2018 | 4/2018–6/2018 | Adjusted P value | ||
| EMS A offload time (min) | 30.87 | 22.08 | 8.789 (1.034) | 0.01 | 16.72 | 15.84 | >0.99 | |
| EMS A offloads <20 min | 130.30 | 300.00 | 169.7 (28.44) | 0.04 | 464 | 489.7 | 0.13 | |
| EMS A offloads <20 min (average %) | 25.80 | 52.40 | 26.6 (3.567) | 0.02 | 68.13 | 68.43 | >0.99 | |
| EMS B offload time (min) | 36.06 | 32.25 | N/A | >0.99 | N/A | N/A | N/A | |
| EMS B offloads <20 min | 23.70 | 36.70 | N/A | 0.82 | N/A | N/A | N/A | |
| EMS B offloads <20 min (average %) | 14.90 | 20.00 | N/A | >0.99 | N/A | N/A | N/A | |
| Boarding hours | 11,070.00 | 6,576.00 | 4,493 (648.7) | 0.03 | 7979 | 5580 | 0.44 | |
| NEDOCS | 141.30 | 114.70 | N/A | >0.99 | N/A | N/A | N/A | |
Offload times shown in minutes per patient. Offloads less than 20 minutes, percent of offloads less than 20 minutes, and boarding hours shown in average per month. National Emergency Department Overcrowding Scores shown in daily average. Analysis performed by Student’s
Results
During the study time period (July 2016–May 2017 and August 2017–June 2018), our ED served 94,735 patients. EMS traffic accounted for 35,505 (37.5%) of all ED patients. EMS A and EMS B traffic accounted for 38.1% and 11.3% of all EMS traffic, respectively. EMS A data for 5,973 patients prior to, and 7,541 patients after, the implementation of the PPFC was analyzed for the time periods of July 2016–May 2017 and August 2017–June 2018, respectively. EMS B data for 2,017 patients prior to, and 1,981 patients after, the implementation of the PPFC was also evaluated.
Following the implementation of the PPFC, we observed a statistically significant decrease in EMS A and EMS B offload times per patient (A: 30.13 versus 24.32 minutes, P<0.0001 and B: 33.67 versus 28.72 minutes, P=0.0007), the number of EMS A but not EMS B offload times less than 20 minutes each month (A: 134.5 versus 315.8, P<0.000001), and the percent of EMS A but not EMS B offload times less than 20 minutes each month (24.51% versus 46.23%, P<0.000001; Figure 1 and Table 2).
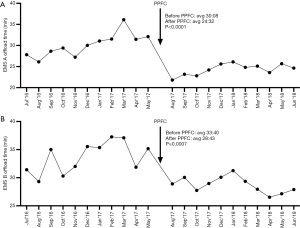
Table 2
| Variable | 07/2016–05/2017 | 08/2017–06/2018 | Difference (SE) | Adjusted P value |
|---|---|---|---|---|
| EMS A total (avg patients per month) | 543.00 | 685.50 | –142.5 (21.09) | <0.0001 |
| EMS B total (avg patients per month) | 183.40 | 180.10 | N/A | >0.99 |
| EMS A + EMS B total (avg patients per month) | 726.40 | 865.60 | –139.3 (28.52) | 0.002 |
| EMS ground traffic (avg patients per month) | 1,503.00 | 1,725.00 | –222.5 (47.51) | 0.003 |
| ED volume (avg patients per month) | 4,116.00 | 4,496.00 | –379.4 (97.53) | 0.02 |
| Boarding hours (avg per month) | 8,439.00 | 7,290.00 | N/A | >0.99 |
| NEDOCS (daily avg) | 118.90 | 147.70 | N/A | >0.99 |
| Admitted patients (avg per month) | 1,481.00 | 1,587.00 | N/A | 0.17 |
| % Admitted patients (avg per month) | 36.00 | 35.30 | N/A | >0.99 |
| % EMS A + EMS B of total EMS ground traffic (monthly avg) | 48.25 | 50.30 | N/A | >0.99 |
| % EMS A of total EMS ground traffic (monthly avg) | 36.07 | 39.84 | –3.772 (0.99) | 0.02 |
| % EMS B of total EMS ground traffic (monthly avg) | 12.18 | 10.46 | 1.726 (0.521) | 0.07 |
| EMS A offload time (min) | 30.13 | 24.32 | 5.815 (0.93) | <0.0001 |
| EMS B offload time (min) | 33.67 | 28.72 | 4.951 (0.94) | 0.0007 |
| EMS A <20 m (offloads per month) | 134.50 | 315.80 | –181.4 (15.37) | <0.000001 |
| EMS B <20 m (offloads per month) | 33.91 | 38.00 | N/A | >0.99 |
| EMS A %<20 m (offloads per month) | 24.51 | 46.23 | –21.72 (2.33) | <0.000001 |
| EMS B %<20 m (offloads per month) | 18.40 | 21.18 | N/A | >0.99 |
Emergency medical services traffic and emergency department volume, emergency medical services percent of traffic, and boarding hours shown in average patients, percent, and hours per month, respectively. National Emergency Department Overcrowding Scores shown in daily average. Offload times shown in minutes per patient. Offloads less than 20 minutes and percent of offloads less than 20 minutes shown in average per month. Analysis performed by Student’s
Given that EMS traffic and ED crowding can influence ED flow and EMS efficiency in the ED, we compared measures of EMS traffic as well as boarding hours per month and NEDOCS before and after the implementation of the PPFC in our ED (Table 2 and Figure 2). Compared to the time period immediately prior to the implementation of the PPFC, we observed a significant increase in the total number of patients per month arriving by all EMS ground traffic (1,503 versus 1,725, P=0.003), patients arriving by EMS B and EMS A combined (726.4 versus 865.6, P=0.002), and patients per month arriving by EMS A (543 versus 685.5, P<0.0001), but not EMS B. Over the study time course, we also observed an increase in the number of patients evaluated each month in the ED (4,116 versus 4,496, P=0.02). We observed no difference in the number of boarding hours per month, the number of patients admitted per month, the percent of patients admitted per month, or in the daily NEDOCS.
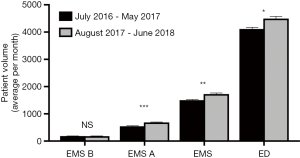
Given that we were only able to calculate offload times for approximately 50% of EMS traffic arriving at our ED, we also determined whether the proportion of patients transported by EMS A and EMS B changed during the time course of this study (Table 2). We observed no change in the percent of EMS traffic arriving by EMS B and EMS A combined. We observed a significant increase in the proportion of patients arriving by EMS A following the implementation of the PPFC compared to the time period prior to the implementation of the PPFC (36.07% versus 39.84%, P=0.02). While not statistically significant, we observed a trend for a decreased proportion of patients arriving by EMS B following the implementation of the PPFC (12.18% versus 10.46%, P=0.07).
Lastly, we sought to calculate the time saved following the implementation of the PPFC. Because inter-hospital transfer of previously stabilized patients comprises a large portion of non-EMS A traffic, whereas EMS A traffic arrives only from local scene calls, ED staff has been instructed to prioritize EMS A turnaround time over that of non-EMS A agencies. In order to account for any discrepancy between EMS A and non-EMS A agencies in calculating time saved following the implementation of the PPFC, we compared EMS A to EMS B offload times for the time periods before and after the implementation of the PPFC. We observed that throughout the duration of the study, EMS A offload times remained significantly less than EMS B offload times (July 2016–May 2017: 30.13 versus 33.67 minutes, P=0.014 and August 2017–July 2018: 24.32 versus 28.72 minutes, P<0.000001; Table 3). In calculating time saved, we suspected that offload times for non-EMS A/B agencies would be similar to that observed for EMS B. Following the implementation of the PPFC, an average of 1,725 patients arrived at our ED each month by ambulance ground traffic. Implementation of the PPPC saved 5.81 minutes per patient for 686 EMS A patients (per month) and 4.95 minutes per patient for 180 EMS B and 859 non-EMS A/B patients (per month), equating to 6 days, 8 hours, 8 minutes, and 43 seconds of time saved each month.
Table 3
| Variable | EMS A | EMS B | Difference (SE) | Adjusted P value |
|---|---|---|---|---|
| Offload times: Pre PPFC (min) | 30.13 | 33.67 | –3.535 (1.18) | 0.014 |
| Offload times: Post PPFC (min) | 24.32 | 28.72 | –4.399 (0.59) | <0.000001 |
Offload times shown in minutes per patient. Analysis performed by Student’s
Discussion
A 2006 Centers for Medicare and Medicaid Services statement warned that the “practice (of delaying EMS patient off-loads) may result in a violation of the Emergency Medical Treatment and Labor Act (EMTALA) and raises serious concerns for patient care and the provision of emergency services in a community” (7). Supporting these concerns, a study by Crilly et al. observed that offload times of 30 minutes or longer were an independent predictor of ED length of stay exceeding four hours (6). In turn, longer ED boarding times are associated with higher in-hospital mortality (9). Thus, hospitals and EDs have implemented a variety of strategies in an attempt to buffer increased ED crowding and utilization.
One proposed solution to ED crowding is the expansion of ED capacity (10). However, the addition of ED beds is an expensive endeavor and does not always result in improved offload times (11). During March of 2016, we implemented a similar strategy by opening the MAU, decreasing the burden of medically admitted patients on our ED. The opening of the MAU appeared to be temporally associated with decreased offload times for EMS-A but not EMS-B. The cause of this discrepancy is unclear.
In a further attempt to decrease EMS offload times at our facility, we created the position of the PPFC and provided this new position with the tools to communicate and coordinate EMS flow in the ED. Importantly, the PPFC further decreased offload times for both EMS A and EMS B, demonstrating additional improvement in both ED flow and ambulance return to service time beyond that observed after opening the MAU. Over the study time course, we observed a significant decrease in offload times, with an average of 5–6 minutes of offload time saved per patient, despite increased measures of EMS traffic and unchanged boarding hours and NEDOCS. These time savings amount to over 6 days of “wall time” saved each month.
Other studies have observed improvement with the implementation of similar positions (12, 13). Halliday et al. found that a Medical Duty Officer improved time spent at the hospital by EMS by approximately 4 minutes (13). The Medical Duty Officer, placed in the communication center, suggested alternative transport destinations in the event of ED overcrowding (13). Ambulance diversion has been used as a method to decompress EDs, allowing EDs to stop the flow of ambulance traffic while they reduce congestion. Diversion, however, has been linked to delays in receiving treatment and increased mortality (14, 15). In contrast, our work suggests that a PFCC, stationed in the ED, may yield similar improvements in offload times while avoiding the dangers of ambulance diversion.
Greaves et al. found that an offload nurse improved time to physician by 4 minutes (12). While it remains unclear whether a nurse in the PPFC position might have resulted in similar time savings, in our health system the employment of a paramedic is less expensive than a nurse. Furthermore, we postulated that having a paramedic in this position would improve handoff communication and strengthen ED rapport with EMS. Silvestri et al. showed that simply employing paramedics in the ED improved ambulance off-load times (16). Similarly, our data indicate that employing a paramedic to coordinate EMS traffic can have substantial beneficial impact on EMS flow in the ED. We suspect that some of the benefit of the PPFC position is a result of the paramedic’s familiarity with the EMS system. Thus, the PPFC is an efficient strategy to improve EMS turnaround time, helping to decompress the overcrowded ED and often over-utilized EMS system.
While we conclude that the implementation of a PPFC is an easy and cost effective intervention to improve ED patient flow and ambulance turnaround time, this study does have limitations. For example, offload times were calculated based on data previously entered into EMS agency’s software platform, the accuracy of which is dependent on the initial documentation by clinical staff. In addition, while we attempted to account for major changes made during our study time period (i.e., the implementation of the MAU) that may have contributed to the observed decrease in ambulance offload times, it is possible that other, unidentified variables influenced these results.
Our dataset was limited because records from non-EMS A/B agencies were unavailable. Given the observed preference in offloading EMS A patients in our ED, we assumed non-EMS A/B agencies and EMS B to have similar offload times. However, it is possible that the offload times of non-EMS A/B agencies may differ substantially from that observed for EMS B. Lastly, this study was conducted at a single nonprofit academic tertiary medical center ED in the Southeastern region of the United States. Therefore, our results may not be applicable to other hospital systems. Additional studies are necessary to confirm this study’s observed benefit of a PPFC in the ED.
Acknowledgments
We thank the Emergency Medical Services personnel of our community for their support in this endeavor.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SQUIRE reporting checklist. Available at http://dx.doi.org/10.21037/jhmhp-20-26
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jhmhp-20-26
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jhmhp-20-26). RAM reports personal fees from ApolloMD, the Emergency Medicine Foundation of the Department of Emergency Medicine at the University of Tennessee College of Medicine at Chattanooga (charitable foundation), the University of Tennessee College of Medicine at Chattanooga (academic institution), Merck (42.618 shares), and Proctor and Gamble (51.27 shares). RB reports personal fees from ApolloMD, the University of Tennessee College of Medicine at Chattanooga, Phoenix Air, Tri-County Community College, and Cherokee County EMS. RB serves as the Medical Director for Disaster Medicine, Prehospital Medicine, MedComm and EROC at Erlanger Medical Center, for the Regional Special Operations Group, RMCC – TN Region 3 Med Communication committee, Hamilton County Emergency Medical Services, Puckett Emergency Medical Services (current medical director, past assistant medical director), Catoosa County Fire and Rescue, Walker County Fire and Rescue, Fort Oglethorpe Fire and Rescue, East Ridge City Fire and Rescue, and serves as a Tactical SWAT Physician for Hamilton County EMS/Hamilton County Sheriff Dept. JC reports personal fees from Erlanger Health System, outside the submitted work; and JC is the Senior Director Emergency Services at Erlanger Health System. SM reports personal fees from ApolloMD and the University of Tennessee College of Medicine at Chattanooga. SM serves as the Chief of the Emergency Medicine for Erlanger Health System and the Chair of the Department of Emergency Medicine at the University of Tennessee College of Medicine Chattanooga. JSW reports personal fees from ApolloMD and the University of Tennessee College of Medicine at Chattanooga and consulting fees from Vapotherm, Inc. JSW sits on the advisory board of Physicians 360. JKG has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Because this study did not involve individual patients or review of patient data, it was not subject to review by the Institutional Review Board.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Health, United States, 2016: With Chartbook on Long-term Trends in Health [Internet]. National Center for Health Statistics (US). 2017. Available online: https://www.ncbi.nlm.nih.gov/pubmed/28910066
- National Hospital Ambulatory Medical Care Survey: 2015 Emergency Department Summary Tables [Internet]. Centers for Disease Control and Prevention and the National Center for Health Statistics. 2015 [cited July 16, 2016]. Available online: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2015_ed_web_tables.pdf
- Forero R, McCarthy S, Hillman K. Access block and emergency department overcrowding. Crit Care 2011;15:216. [Crossref] [PubMed]
- Trendwatch Chartbook 2018: Trends affecting hospitals and health systems [Internet]. American Hospital Association. 2018 [cited July 16, 2016]. Available online: https://www.aha.org/guidesreports/2018-05-22-trendwatch-chartbook-2018
- Carter AJ, Overton J, Terashima M, et al. Can emergency medical services use turnaround time as a proxy for measuring ambulance offload time? J Emerg Med 2014;47:30-5. [Crossref] [PubMed]
- Crilly J, Keijzers G, Tippett V, et al. Improved outcomes for emergency department patients whose ambulance off-stretcher time is not delayed. Emerg Med Australas 2015;27:216-24. [Crossref] [PubMed]
- EMTALA - "Parking" of Emergency Medical Service Patients in Hospitals [Letter written July 13, 2006 to State Survey Agency Directors] [Internet]. Centers for Medicare and Medicaid Services and the Department of Health and Human Services. 2016 [cited July 16, 2016]. Available online: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/downloads/SCLetter06-21.pdf
- Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf 2016;25:986-92. [Crossref] [PubMed]
- Singer AJ, Thode HC Jr, Viccellio P, et al. The association between length of emergency department boarding and mortality. Acad Emerg Med 2011;18:1324-9. [Crossref] [PubMed]
- Silvestri S, Ralls G, Papa L, et al. Impact of Emergency Department Bed Capacity on Emergency Medical Services Unit Off-load Time. 2006 SAEM Annual Meeting Abstracts. Acad Emerg Med 2006;13:S70-1.
- Crilly JL, Keijzers GB, Tippett VC, et al. Expanding emergency department capacity: a multisite study. Aust Health Rev 2014;38:278-87. [Crossref] [PubMed]
- Greaves T, Mitchell M, Zhang P, et al. The impact of an Emergency Department ambulance offload nurse role: A retrospective comparative study. Int Emerg Nurs 2017;32:39-44. [Crossref] [PubMed]
- Halliday MH, Bouland AJ, Lawner BJ, et al. The Medical Duty Officer: An Attempt to Mitigate the Ambulance At-Hospital Interval. West J Emerg Med 2016;17:662-8. [Crossref] [PubMed]
- Yankovic N, Glied S, Green LV, et al. The impact of ambulance diversion on heart attack deaths. Inquiry 2010;47:81-91. [Crossref] [PubMed]
- Pham JC, Patel R, Millin MG, et al. The effects of ambulance diversion: a comprehensive review. Acad Emerg Med 2006;13:1220-7. [Crossref] [PubMed]
- Silvestri S, Sun J, Gutovitz S, et al. An Emergency Department Paramedic Staffing Model Significantly Improves EMS Transport Unit Offload Time – A Novel Approach to an ED Crowding Challenge. Emerg Med: Open Access 2014;4(6).
Cite this article as: Martin RA, Buchheit R, Carman J, Gray JK, Mendiratta S, Whittle JS. A paramedic patient flow coordinator improves ambulance offload times in the emergency department. J Hosp Manag Health Policy 2020;4:21.

