
Translation of policy and guidelines into practice: lessons learned from implementation of the Cancer Pain Management Guideline
Introduction
World Health Organization announced that cancer is one of the most significant diseases, given its high leading cause of death and impacts of the increasing annual global economic cost of health services (1). The International Agency for Research on Cancer reported that 14.1 million people in the world have new diagnoses of cancer (of all types, except non-melanoma skin cancer) and that 32.6 million people were living with cancer over the last 5 years of their lives in 2012 (2). Of concern, within the current report of the National Cancer Institute was an estimate that there would be a 50% incremental increase in rate of cancer cases worldwide between 2012 and 2030 (3). Stewart and Wild in their report for the WHO reported that South Korea has one of the highest cancer incidence rates in the world (4): The prevalence of cases has increased from 1,370,049 to 1,464,935, despite the decreased incidence rates. They attributed these rates to the increased survival rates (5,6).
With the high prevalence of cancer and increased survival rates, cancer pain has become an ongoing challenge for patients, families, healthcare professionals including nurses and the society. Pain can occur at any stage of the disease, arising from the cancer itself, from pre-existing conditions and from the aggressive cancer treatment regimens associated with chemotherapy, radiotherapy and surgery. Increasing cancer prevalence rates means increasing the chances of pain experience among those patients with cancer, this in turn decreases the quality of life for the patients and those around them (7-10). This is evident in the international literature. In a systematic review and meta-analysis of 122 international studies (11), the pain prevalence rate was between 39.3% (post curative treatment) and 66.4% (current advanced, metastatic, or terminal disease). This figure is similar in South Korea in that 38.4% of cancer patients report suffering from pain and 10.6% of cancer patients experience severe pain (12).
Research particularly shows that unresolved pain can lead to negative patient outcomes among those patients with cancer (13,14). Inadequate pain management decreases quality of life by impacting on levels of daily activities and sleep. It increases the risk of medical complications associated with the use of analgesic medications, such as constipation and drowsiness resulting in refusal of treatment. In addition, the presence of unrelieved cancer pain could increase the burden of disease for Korea and other nations because of increasing lengths of stay in hospital and readmission rates (15). The relief of cancer pain is recognized as the most significant issue in cancer care and a key area for improvement in order to enhance quality of life among the patients with cancer and their families (16) in both national and international contexts.
Given the importance of adequately managing pain among those patients with cancer, different countries have developed and implemented guidelines to achieve evidence-based practice (EBP) to improve quality of patient outcomes (17-19). In South Korea, the ‘Cancer Pain Management Guideline (CPMG)’ was developed in 2004 following the many concerns of healthcare professionals, including nurses, about the pain and suffering of patients with cancer and has been encouraged to use over the last 15 years. Originally the rational for guideline development arose from reviews of the WHO Cancer Pain Relief document, which drove the policy and calls to achieve consensus on managing the needs of those people with cancer pain and initiate systematic research for evidence on approaches to more effective pain management (20,21). There were 25 academic groups that participated in developing and updating the CPMG and the Korean Society of Nursing Science and the Korean Oncology Nursing Society were the two nursing ‘academic groups’ involved (22).
The development of the CPMG was an integral part of the changes that Korean society was experiencing in an effort to improve the quality of care provided within the healthcare system. The CPMG has been reported as the precursor to major changes in cancer pain management practices, and has been the only evidence-based guideline (EBG) existed for more than a decade in South Korea, particularly in terms of the use of pharmacological interventions (7). However, there were only limited number of studies that showed the uptake of the CPMG, and the impact on cancer pain management practices especially for the nurses who provided direct care for patients with cancer (23,24). Given the central role that nurses play in providing care for patients with pain related to cancer and its treatment, it was critical to investigate the introduction/implementation of the CPMG and the relevant factors that could have influenced on implementations of the CPMG. Therefore, this paper aims to report on whether the CPMG has been implemented among the nurses who provide care for those patients with cancer in these particular study settings. Any findings on influential factors impacting implementation of the guidelines are included.
Methods
Design and conceptual framework of the study
Critical ethnography (CE) underpinned the study design and the framework of Greenhalgh, Robert, and Bate’s ‘A Conceptual Model for the Spread and Sustainability of Innovations in Service Delivery and Organization’ (see Figure 1) guided the data analysis (25). This unifying conceptual model was based on a systematic review of empirical research studies and was used to identify the determinants of diffusion, dissemination and implementation of innovations in healthcare service delivery and organization. The spread of an innovation such as the introduction of guidelines requires analysis of complex interactions among the different elements of the conceptual framework. The relevant elements include:
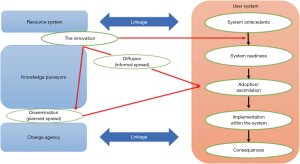
- The innovation: Development and publication of the CPMG in South Korea was an innovation at the time of its introduction. There were no national guidelines that could help either healthcare professionals or non-healthcare professionals including government officials and the public prior to the publication of the guidelines to understand cancer pain management better;
- Adoption: Rogers (26) particularly defined adoption as ‘the decision to make full use of the innovation as the best course of action available (p. 21)’. Greenhalgh et al. emphasize that people actively seek innovations to experiment with, evaluate, find meanings in, challenge, complain about and modify: the nature of this adoption process makes the whole process complex (25);
- Assimilation through diffusion and dissemination: once adopted, an innovation has to be spread by the process of communicating the innovation outside the original system (27). In particular, spreading the innovation within a team, unit, department and/or organization is called assimilation of the innovation. Whilst dissemination is defined as a planned, formal and centralized way of spreading innovation through vertical hierarchies, diffusion is defined as an unplanned, informal and decentralized way of spreading innovation through more horizontal and peer-mediated routes (26-28);
- Inner context: although, spreading the innovation might initially begin with individuals, it should eventually occur systematically, throughout the ward and the organization. Hence, it is important to consider the impact of organizational context in order to enhance the spread of the innovation following it becoming a routine within the system. The contextual variables that indicate greater likelihood for adoption of the innovation include the structure of the organization, absorptive capacity for new knowledge, and receptive context for change (25);
- Outer context: the decision on adopting the CPMG by a group of nurses can be influenced by aspects of the outer context such as inter-organizational norms and values, and collaboration (25).
Ethical approval
Approval was obtained from the University of Newcastle Human Research Ethics Committee (H-2012-0071) and the Daehan University Medical Center (DHUMC) (Pseudonym) IRB (ECT 13-12-08) before entering the field to conduct the study. All participants provided informed consent.
Research setting and participants
The study setting, DHUMC in South Korea is a tertiary teaching hospital in the capital city, Seoul, with 850 beds. DHUMC has been a facility for patient care and also dedicated to education, research and treatment for a long time. It has several departments including hematology and oncology, and three units that mainly provided care for cancer patients, hence those units were invited to participate in the study.
The inclusion criteria for participants included the RNs who (I) had cancer care experiences of more than 3 years; (II) were directly involved in care of patients with cancer who were experiencing pain; (III) were permanently employed on the study unit.
Exclusion criteria: the RNs who worked in pediatric settings.
Data collection
Permission to conduct the study was granted by the Direct of Nursing (DON) and three Nurse Unit Manager (NUMs) and a Nurse Educator (NE). A total of 16 RNs from 3 units in the DHUMC attended the information session about the study and 11 RNs consented to participate in the study. However, one RN withdrew from the study, because of early delivery of her baby. Table 1 presents the demographic characteristics of the RN participants.
Table 1
| RN’s name (initial) | JN | ES | JH | EN | YH | MH | JM | KM | NR | YS |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | F | F | F | F | F | F | F | F | F | F |
| Age (year) | ~30 | ~30 | ~30 | ~40 | ~30 | ~30 | ~30 | ~35 | ~30 | ~30 |
| Length of working as a RN (year) | ~5 | ~10 | ~10 | ~20 | ~10 | ~10 | ~10 | ~5 | ~10 | ~10 |
| Length of cancer care (year) | ~5 | ~10 | ~10 | ~15 | ~10 | ~10 | ~10 | ~5 | ~10 | ~10 |
| Employment status | FT | FT | FT | FT | FT | FT | FT | FT | FT | FT |
| Education status | B | D | D | MP | D | D | MP | D | D | D |
| Cancer pain management experience | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Awareness of the CPMG | N | N | N | N | Y | N | N | N | Y | N |
F, female; FT, full time; PT, part time; D, diploma; B, bachelor; MP, master in progress; Y, yes; N, no.
The data collection methods for this study included: (I) participant observation; (II) in-depth semi-structured interviews, and (III) document analysis. The primary author of this paper conducted 7 months of participant observation and in-depth semi-structured interviews.
The focus of participant observation was to gain a holistic understanding of the experience of participants, the practice culture and context. Participant observation of care delivery preceded the interview in most cases, and reviews of the relevant documents were maintained throughout the observation period. Participant observations reporting included structural and organizational features of each unit and the participants’ activities and dialogue, if the researcher considered these were relevant.
Each of the 10 semi-structured interviews took approximately an hour in a quite meeting room using an open-ended interview schedule, which was developed based on the literature review, and research aims and questions. The researcher was taking detailed notes while listening, but was mindful of balancing between attentive listening and note taking. Interviews were recorded and transcribed verbatim.
Documents included in analysis included the Nursing Task Guidebook (NTGB), patient information sheets and the Electronic Medical Record (EMR)/Electronic Nursing Record (ENR). The researcher focused on answering questions such as “Are there any formal EBGs (e.g., CPMG) that drive nursing practice for caring cancer patients with pain?” “Are these guidelines on an international level? In what way or to what extent are they so?” and “Is nursing practice for cancer pain management consistent (or inconsistent) with the guidelines? In what ways or to what extent is this so?”
Data analysis
The primary author was involved in transcribing the first two sets of interview data to be familiar with the data set and the process of analysis and another eight sets of interview data were transcribed by a transcriptionist who signed for confidentiality agreement. She read the data for several times with noting initial ideas and developed 10 storylines about each 10 RN. Open coding was conducted to generate initial codes across the entire data set with application of critical lenses such as use of particular language, context-situation and culture, and meaningful moments. Data relevant to each code was generated. Codes were compared and sorted into potential themes, then the themes were reviewed to generate a thematic ‘map’ of the analysis. The primary author conducted ongoing analysis to refine the specifics of each theme and their relationship to each other and ‘the fit’ with a broader overall story in relation to the research questions. After the iterative processes, themes emerged from the analysis based on significant statement highlighted in the data during the process of reviewing and responding to the research aims and questions. Themes and relationships were scrutinized at each stage by the other authors to ensure accurate interpretation and credibility (29).
Results
Table 2 presents 3 themes, 6 subthemes, data sources and quotations.
Table 2
| Theme | Subtheme | Data source | Quotations |
|---|---|---|---|
| Seeds of innovation | Guidelines for nursing practice | Participant observation, document analysis, interview | The ‘NTGB’ included four different pain measurement scales that nurses could use for the patients in different circumstances as follows; NRS (Numeric Pain Rating Scale), PAFS (Pain Affect Faces Scale), NIPS (Newborn Infant Pain Scale), and FLACC (Face-Legs-Activity-Cry-Consolability Scale). According to the NTGB, nurses were required to assess the patients’ pain intensity, location, pattern, frequency and duration by using the pain scales; record the nursing intervention; report to the doctors, if there was any unrelieved pain after interventions; and provide adequate education about pain to patients and families (Field note, summary of NTGB) |
| We do have a guideline (NTGB) to train the new graduates and also the checklists...//…we have one in the unit and every new graduate has a guidebook (NTGB) (Jinhee) | |||
| There is a hospital policy that has been set. I mean, we attend to pain assessment once every shift…and enter pain score (in the EMR system)//(it doesn’t matter if patients have pain or not) we attend (to checking of pain scores) as a routine (Eunsoo TC3) | |||
| Lack of receptivity for change | Interview | The atmosphere of the hospital is not something like (someone would want to initiate any ideas/practice), but just take orders and to do it (follow the order).//…it (trying to initiating the ideas/practice) could be another example of behaviour (that is trying to) draw people’s attention (because the one who initiates the ideas/practice would ‘stand out’ and people would recognise her/him)…//we don’t really like it (behaviour that draws people’s attention) (Jinhee C-VII-3) | |
| I think I might have been working without much attention to manage pain and…when I was invited to participate in this study, I responded in a negative way. I (even) said to the Head Nurse “Do I really have to do this much?” and she said jokingly “That’s why you don’t grow (within your profession).” (Nari) | |||
| I hardly talked with the Head Nurse. She’s a little bit hard to face…(Jinhee C-VII-5) | |||
| Resources for the management of pain | Interview, participant observation | For example, of hot bag, we don’t have hot bag…Also, massage…there is equipment that the volunteers bring in, but we don’t have our own massage equipment or things like that…(Jina A-VII-19)…we used (hot bags) pouring hot water in it, but it had a risk of burn, so we can’t use it anymore (Jina TC17) | |
| It would be better to have professional (therapists) for those music or art (therapies) than us, but that there is no one who could come…(Jina A-VII-20) | |||
| We have music played in a music therapy room…meant to provide emotional support and make people relax. Patients said it is really helpful to be in that room to listen to the music. So we made the room, but now…we often even don’t play the music. If we got really busy in the morning, we forgot to turn the music on…(Eunah D-VII-12) | |||
| Well…because of busyness (I can't do adequate pain management)…busyness and also because patients are sick and…I think it’s because of busyness.//Just the shift itself (makes me being busy) too many surgeries, admissions, (managing) post-op patients, (managing) new admissions and make discharges and solve the issues when patients make complaints in between (Eunsoo, B-VII-4) | |||
| There are many activities like art therapy and music therapy…I couldn’t use them although I knew them, because I was neither a professional (instructor) for those therapies nor had a certificate for it, so I didn’t know much about it (Younhee TL40). | |||
| CPMG: Stimulus for changes | Hospital accreditation | Participant observation, interview | I think it (hospital accreditation) is quite effective. It has the marketing effect (given) that we have achieved JCI accreditation, in this country…this is one of the few hospitals that achieved the foreign JCI accreditation…I’ve heard that we’ve got increased numbers of patients, since the accreditation (Miho F-IX-4) |
| The (hospital) system has been totally changed and there has been more work done electronically (Miho F-IX-4) | |||
| ‘All patients are screened for pain and assessed when pain is present’—I found in the JCI accreditation guideline under the section patient access and assessment that pain screening and assessment are specifically stated (Field note, Miho). | |||
| The hospital started using the EMR for the purpose of the JCI accreditation. Nurses now had more frequent checks on for the patient, but Eunah was not sure whether it was worthwhile to keep recordings such as completing frequent ‘Pain Report’ and thus have less time to provide hands on care (Field notes: Eunah) | |||
| We (the hospital) wanted to show off to patients that we’ve gone through the accreditation and achieved it in order to promote its reputation, so I think (preparation for accreditation and changes in the hospital) was organised without clear plans…(Miho) | |||
| No, I don’t usually ask the question as in number…but (I used) the number during the accreditation (period)…//Really…It’s been about 6 years, but probably I’ve only asked with numbers less than 10 times…//During the accreditation…When the JCI came (to assess for the accreditation), we actually went and asked the patients with numbers (physically attend the patients to assess pain with numeric pain scale), how much pain they had, because we were told that they (the auditor) would also go and ask the patients (if we had come to assess pain with the scale) (Younhee E-VII-9) | |||
| Changes in leadership, changes in practice | Interview | The biggest reason (of the changes in not using much placebo) would be the professors, because there has been changes in what they think. Previously (the professor) didn’t pay much attention on such problem (pain issue). Well…but now they’ve been taking (the issue of) pain really seriously. Therefore, if a patient complains of pain, they do their best to (reduce pain)//And Professor OOO has become the Director of the Medical Centre, hasn’t she? She has been (involved in) hospice…And I think it (Professor OOO and her involvement in hospice care) was the reason why we have a hospice team (Miho) | |
| CPMG: Diffusion & dissemination | “We don’t know much about it.” | Interview | There is a guideline for use of opioid, isn’t there? Something like you use it (this guideline) like this in this situation and if it’s (use of certain opioid analgesic is) not working, use something else…like this…But actually, we don’t know much about it (the CPMG) (Nari I-VI-1) |
| I visit the patients, once I have handover…and if I have enough time, I start asking questions to the patients (who are) on the first or second day of post-operation. (Jeongmi G-I-1) |
Seeds of innovation
The observations of nurses interacting with patients suggested there was little evidence of use of the CPMG; instead the nurses were using NTGB.
Guidelines for nursing practice
The NTGB was the major source of directions for all nursing practice including pain management of patients with cancer as part of their comfort and care. It was noted during observation and review of the relevant documentation that there was limited evidence of adequate information or directions with rationales for nurses to make decisions within their practice for managing cancer pain. For example, although the nurses followed the NTGB that provided instructions about nursing practice, the content was very limited, especially around descriptions of interventions for pain. The content of the NTGB did not mention levels of evidence and nursing perspectives; they simply instructed nurses to perform the task of managing pain within medically driven structures and processes.
Lack of receptivity for change
A lack of receptivity to change was attributed to the organizational constraints to innovation in practice. Strong leadership from managers, those who are supportive in adopting the innovation and have good relations with the nurses are considered important elements in creating receptive contexts for change. On the other hand, an embedded hierarchical relationship among nurses was apparent; this minimal openness and a non-receptive culture limited chances for communication among the nurses. Support should be in place for adoption of the CPMG in nursing practice to improve cancer pain management. However, such support was not reported or observed in this study.
Resources for the management of pain
In order to use different interventions to provide individualized care in managing pain for those patients with cancer, nurses needed to have sufficient levels of support. Despite the positive effects of extra material resources that could increase the chance of spreading and sustaining the CPMG, the participants often reported limited availability of resources. A lack of equipment supplies for non-pharmacological interventions such as hot bags was reported in two Units. Safety reasons were cited for the removal of hot bags from healthcare settings without replacement with safe alternatives such as heat lamps. In addition, human resources who could provide a variety of non-pharmacological interventions including professional therapists were reported to be limited, despite their effectiveness of enhancing pain management outcomes. Some interventions such as art therapies that were known as effective could be more complex in terms of instruction, thus needing professional instructors. However, as there was no internal and/or external access to professional instructors, the nurses appeared to believe that there was nothing much that could be done. On the other hand, it was reported and observed that even providing a simple level of music therapy was often ignored due to a busy workload with insufficient staffing in one of the Units, where there was a music room. Although, some RN participants appeared to have learned about certain non-pharmacological interventions in their practice, they often lacked confidence about its use in nursing practice, noting they were not certificated for this. It became apparent that even if the CPMG were introduced, optimum outcomes from the adoption of the CPMG would not be achieved, if nurses’ choices on interventions were limited due to inadequate resource support or confidence to use the resources they had.
CPMG: stimulus for changes
In the study contexts, it appeared that any tension for changes in managing pain did not arise from the individual nurse’s reflection on their own practice. Instead, it was externally mediated because of the hospital accreditation and changes in a medical consultant’s attitudes towards cancer pain management.
Hospital accreditation
The study hospital setting is one of the few tertiary education hospitals in Korea accredited by the Joint Committee International (JCI). The aim of the accreditation system is to improve patient-safety and quality of health care, and promote rigorous standards of care and achieve optimal levels of performance. Hence, all study sites were formally recognized as quality healthcare settings once the JCI accreditation was achieved; this consequently could enhance their reputation. The RN participants reported that the accreditation process influenced the introduction of some changes in this healthcare setting such as introduction of the EMR system, which was an innovation in itself. The hospital installed computers with programs to support patient care systems. This in turn led to change in nursing practices such as maintaining a ‘Pain Record’ that in turn mandated regular pain screening/assessment as a routine.
In theory, the tension for change imposed by the accreditation and the consequent changes in the use of ‘Pain Record’ in the EMR, demonstrated readiness for the uptake of other innovations such as the CPMG. However, the participant nurses considered changes in their practice arising out of accreditation as suboptimal; they were frustrated and pessimistic. They considered the accreditation requirements and processes caused too much indirect activity for them (i.e., recording of what they did during their shift) and that this reduced time for direct nursing care. The changes in nursing practice resulting from the hospital accreditation without nurses’ understanding of changes increased doubt amongst nurses about its value in relation to patient care and pain management.
Irrespective of the Unit, given the nurses’ perceptions about the value of the accreditation and the changes to practice, any changes seemed to reflect a ‘temporary performance’ rather than achieving sustained changes in practice aiming for better nursing care in managing pain. Regardless of understanding the purpose of accreditation, the nurses said it was important to comply with the accreditation criteria, but it did not change the quality of their long-term practice including pain management.
One can see from the above that the nurses in the study were frustrated about the demands for the level of care that they were expected to meet, and pessimistic about the influence of accreditation on their own practice and patient outcomes without sufficient resources. The absence of the use of CPMG in their practice to manage pain among the patients with cancer was apparent, so was the frustration and pessimistic attitude toward accreditation.
Changes in leadership, changes in practice
Another indicator of tension for change was noted when there was a change in medical leadership, which influenced approaches to the management of cancer pain and increased use of analgesics. A newly appointed medical consultant with experience in hospice care meant that the use of placebo, previously a common practice in this setting, was almost abolished. Miho noted the change of attitude towards pain management from the new vice-president of the hospital and this meant changes in the overall medical team’s approach to cancer pain management. The Medical Officers (MOs) used less, almost no placebos since the vice-president of the hospital was also the consultant of the hospice team and her views heavily influenced pain management in the unit. The role of the Director of the medical center heavily influenced the practices of not only MOs, but also nurses. Such changes in leadership were a positive step towards possible changes in nursing practices.
CPMG: diffusion and dissemination
“We don’t know much about it”
Only one nurse in the study acknowledged the existence of the CPMG, but even though the Center in which she worked promoted itself as excellent in treating cancer including symptom management of pain. She did not use the guidelines in reference to her own practice. This ignorance of the CPMG was acknowledged by the participant and also observed by the researcher; the nurses’ practices of attending to pain screening/assessment often depended on whether the nurses felt they had enough time to do so during the rounding rather than according to the CPMG, which recommended frequent screening and comprehensive assessment.
Discussion
Providing nursing care for those patients with cancer in managing pain based on evidence has become critical, because EBP can improve the quality of care and patient outcomes (16). As pain is an individual patient experience, nurses who provide care for those patients with cancer are required to develop their ability to make clinical decisions for those individuals using the best evidence that reflects the particular patient’s situation (30). However, the findings illustrate the limited extent to which nurses were informed about, or adopted, the national guidelines for cancer pain management. The introduction and implementation of the CPMG was not evident, and there was no evidence of innovations in nursing practice around pain management for cancer patients existed. Instead, nurses used the NTGB which was clearly limited in terms of providing directions for nurses reliant on a full suite of roles and functions around pain management for those patients with cancer. The findings in this study show professional and organizational related factors that have influenced on implementation of an innovation, CPMG, in managing cancer pain.
First of all, absorptive capacity for new knowledge around the innovation as a contextual variable in inner context could be affirmed by a work culture that used guidelines in nursing practice, the NTGB to optimize the quality of care and patient outcomes although its quality was limited yet as an international level of EBGs. Receptiveness for change among nurses and the organization is another important contextual variable in inner context, as adopting an innovation like the CPMG would require every individual nurse to make some changes in their practice. However, in this study setting, achieving international accreditation was essential and the focus of the organization, given the recognition of the need for proof of the quality processes and outcomes within the healthcare system. Accreditation could have been a crucial opportunity to introduce and implement the CPMG as EBGs and to improve care quality, however nurses in this setting did not see that the accreditation achieved improvement in care quality inclusive of nursing practice.
Secondly, the above could be attributed to the fact that the purpose of the changes to achieve international accreditation was not clearly set up by the organization and/or communicated to the nurses as improvement of care quality and patient outcomes. There has been no shared understanding about the achievement of accreditation and the use of CPMG as the way of improving care quality in caring for patients with cancer who are experiencing pain. This degree of change demands a work climate that is receptive to challenges but supportive through any change process (25). However, the analysis of the findings has revealed an absence of evidence of the organization’s role in support of CPMG and subsequent support for quality care and workplace culture making. The findings also indicated that potential barriers such as the atmosphere and structure of the organization did not support the initiation of new ideas and practices, and led to limited support in resources, both human and material. Although there were some reports of positive changes in cancer pain management among MOs influenced by practice changes among the medical leadership, tension for changes in managing pain among nurses was externally mediated by their participation in and achievement of accreditation in the study setting. Despite the reports of several advantages of achieving accreditation including improvements in care processes and use of information (31,32), the negative influences of accreditation prevailed. The changes have not been sustained after the achievement of the accreditation, despite the initiation of changes at the organizational level. This has implications that any changes including the implementation of accreditation and use of CPMG for promoting care quality and patient outcomes warrant organizational commitment to adequate initial and ongoing resource support.
Another area that revealed insufficient support from the organization was apparent in the reports of shortages of human resources. Perceptions of excessive workload due to insufficient staffing is one of the most frequently and extensively reported barriers in all areas of nursing including in this study setting. Jun, Kovner, and Stimpfel emphasize that excessive workload causes nurses to be hindered in the use of recommended guidelines regardless of their recognition of their advantage in patient outcomes, because they struggle with completing routine tasks (33). Obtaining adequate levels (in quality and quantity) of nurse staffing can reduce possible issues with nurses’ functions of monitoring and early detection of problems such as pain and pain related issues (34). The excessive workload may not be an issue that can be solved with a simple strategy, but it should be considered as one important element in a range of inevitable contributors to limited care outcomes in cancer pain management through the use of EBGs.
This study was conducted in three different units in one acute hospital setting. Therefore, the findings need to be interpreted with caution. Only ten RNs were included in the study. However, they were a representative sample in terms of their ages and experiences. In addition, the final sample size of ten RNs was adequate and enabled data saturation to fully analyze the topic under investigation. The study has identified in-depth views and beliefs of nurses in managing cancer pain. Multiple additional perspectives including those of patients, families and MOs will be useful to add further insights into optimal cancer pain management.
Conclusions
The findings show potential relevant factors, particularly professional and organizational related factors that have influenced implementation of the innovation, the CPMG to manage cancer pain, if and where it has been introduced. Although there were positive elements such as strong leadership from the managers, negative elements were revealed including organizational constraints to innovation, an embedded hierarchical relationship among nurses and limited choice of resources. Additionally, the findings revealed that external stimulus for changes including hospital accreditation and changes in medical leadership could make some changes in nursing practice, but it might not guarantee changes in quality of long-term nursing practice.
The organization could take several roles in implementing an innovation, the use of CPMG in nursing practice including creation of a workplace culture which is receptive to and supportive of the implementation of CPMG in nursing practice, provision of an adequate level of necessary human and material resources, and understanding of the purpose of adopting the innovation, which should focus on improving the quality of care and patient outcomes before promoting organizational reputation, as the latter could be achieved once the quality of care is enhanced.
Acknowledgments
Funding: This work was supported by an Australian Government Research Training Program (RTP) Scholarship for M. Kim’s PhD scholarship. PhD host was the University of Newcastle. Funders had no involvement in the study design, analysis, manuscript preparation or decision to submit for publication.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jhmhp.2020.02.01). This work was supported by an Australian Government Research Training Program (RTP) Scholarship for M. Kim's PhD scholarship. PhD host was the University of Newcastle. Funders had no involvement in the study design, analysis, manuscript preparation or decision to submit for publication. SJ serves as an unpaid editorial board member of Journal of Hospital Management and Health Policy from Sep. 2019 to Aug. 2021.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Approval was obtained from the University of Newcastle Human Research Ethics Committee (H-2012-0071) and the Daehan University Medical Center (DHUMC) (Pseudonym) IRB (ECT 13-12-08) before entering the field to conduct the study. All participants provided informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organisation. Cancer Geneva: World Health Organisation. Available online: http://www.who.int/mediacentre/factsheets/fs297/en/
- International Agency for Research on Cancer. GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. Available online: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx
- National Cancer Institute. Cancer statistics. Available online: https://www.cancer.gov/about-cancer/understanding/statistics
- Stewart BW, Wild CP. World cancer report 2014. Lyon: International Agency for Research on Cancer, 2014.
- Jung KW, Won YJ, Kong HJ, et al. Cancer statistics in Korea: Incidence, mortality, survival and prevalence in 2012. Cancer Res Treat 2015;47:127-41. [Crossref] [PubMed]
- Jung KW, Won YJ, Oh CM, et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat 2017;49:292-305. [Crossref] [PubMed]
- Lee SC. Management of cancer pain in Korea. Eur J Pain Supplements 2007;1:6-9. [Crossref]
- World Health Organisation. Cancer fact sheet. Available online: http://www.who.int/mediacentre/factsheets/fs297/en/
- Neufeld NJ, Elnahal SM, Alvarez RH. Cancer pain: a review of epidemiology, clinical quality and value impact. Future Oncol 2017;13:833-41. [Crossref] [PubMed]
- Onsongo LN. Barriers to cancer pain management among nurses in Kenya: A focused Ethnography. Pain Manag Nurs 2019; [Epub ahead of print]. [PubMed]
- Van den Beuken-van Everdingen MHJ, Hochstenbach LMJ, Joosten EAJ, et al. Update on prevalence of pain in patients with cancer: Systematic review and meta-analysis. J Pain Symptom Manag 2016;51:1070-90.e9.
- Hong SH, Roh SY, Kim SY, et al. Changes in cancer pain management in Korea between 2001 and 2006: Result of two nationwide surveys. J Pain Symptom Manage 2011;41:93-103. [Crossref] [PubMed]
- Kenzik K, Pisu M, Johns SA, et al. Unresolved pain interference among colorectal cancer survivors: implications for patient care and outcomes. Pain Med 2015;16:1410-25. [Crossref] [PubMed]
- Elliott E. Psychological impact of cancer pain on patients and their quality of life. Br J Nurs 2014;23:805-8. [Crossref] [PubMed]
- Brink-Huis A, van Achterberg T, Schoonhoven L. Pain management: A review of organisation models with integrated processes for the management of pain in adult cancer patients. J Clin Nurs 2008;17:1986-2000. [Crossref] [PubMed]
- Choi M, Kim HS, Chung SK, et al. Evidence-based practice for pain management for cancer patients in an acute care setting. Int J Nurs Pract 2014;20:60-9. [Crossref] [PubMed]
- Scottish Intercollegiate Guidelines Network. Control of pain in adults with cancer: A national clinical guideline. Available online: www.sign.au.uk
- NHS Quality Improvement Scotland. Best practice statement-The management of pain in patients with cancer. Available online: http://www.healthcareimprovementscotland.org/previous_resources/best_practice_statement/cancer_pain_management.aspx
- National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Adult cancer pain. Available online: https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf
- Cancer pain management guideline. 4th ed. Seoul: Ministry of Health and Welfare, 2010.
- Heo DS. Development of cancer pain management guideline in Korea. J Korean Soc Qual Assur Health Care 2007;13:29-33.
- Cancer pain management guideline. 5th ed. Seoul: Ministry of Health and Welfare, National Cancer Center 2012.
- Cho EK. Nurses' knowledge and performance of cancer pain management. Daegu: Keimyung University, 2009.
- Yu HJ. Hospice ward and medical ward nurses' knowledge and performance of cancer pain management. Seoul: Hanyang University, 2011.
- Greenhalgh T, Robert G, Bate P. Diffusion of innovations in health service organisations: A systematic literature review. Chichester: Wiley, 2008.
- Rogers EM. Diffusion of innovations. 4th ed. New York: Free Press, 1995.
- Guideline on spread and sustainability. Edinburgh: Healthcare Improvement Scotland 2013.
- Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organisations: Systematic review and recommendations. Milbank Q 2004;82:581-629. [Crossref] [PubMed]
- LoBiondo-Wood G, Haber J. Nursing research: Methods and critical appraisal for evidence-based practice. 7th ed. Missouri: Mosby Elsevier 2010.
- Eaton LH, Meins AR, Mitchell PH, et al. Evidence-based practice beliefs and behaviours of nurses providing cancer pain management: A mixed methods approach. Oncol Nurs Forum 2015;42:165-73. [Crossref] [PubMed]
- El-Jardali F, Jamal D, Dimassi H, et al. The impact of hospital accreditation on quality of care: Perception of Lebanese nurses. Int J Qual Health Care 2008;20:363-71. [Crossref] [PubMed]
- Yoon J. Effects of nurses' awareness of healthcare accreditation system on medical service quality and nursing performance. Seoul: Hanyang University of Korea, 2015.
- Jun J, Kovner CT, Stimpfel AW. Barriers and facilitators of nurses’ use of clinical practice guidelines: An integrative review. Int J Nurs Stud 2016;60:54-68. [Crossref] [PubMed]
- Brooten D, Youngblut JM. Nurse dose as a concept. J Nurs Scholarsh 2006;38:94-9. [Crossref] [PubMed]
Cite this article as: Kim M, Jeong S, McMillan M, Higgins I. Translation of policy and guidelines into practice: lessons learned from implementation of the Cancer Pain Management Guideline. J Hosp Manag Health Policy 2020;4:12.

