
Introduce new paper-based outpatient morbidity recording system to outpatient departments of public hospitals in Sri Lanka: feasibility study
Introduction
Health status is often measured using a range of indicators of mortality and morbidity. Morbidity refers to diseases, illness, injuries and disabilities in a population. Furthermore it provides vital feedback in setting priorities of health system reforms (1). Morbidity data derived from Health Management Information Systems (HMIS) describe the real burden of disease in a community. A continuous morbidity registry provides data for longitudinal clinical research in general practice. Accuracy and consistency of the health records are crucial to ensure in sound management of health system resources (2).
Health care services in Sri Lanka are provided through both public and private sector. Although, the bulk of the in-ward patient service (90%) is provided from the government hospitals, the outpatient services are almost equally shared (50%) among two sectors (3). By the end of 2015, there were 1,104 curative care hospitals governed by Ministry of Health Sri Lanka. These government hospitals have been providing services to average 50 million out-patients per annum (4). These facilities include range of primary, secondary and tertiary care provided with Out Patient Department (OPD) services with or without in-patient facilities.
Morbidity data of patients attending the OPD are not routinely recorded and collected in public sector hospitals in Sri Lanka (5). Morbidity data is recorded only for patients seeking treatment as inward-patients of government hospitals. Hospital in-patient and out-patient records in local settings are not comprehensive enough to assess the prevalence of most of the common diseases (6). National morbidity statistics in HMIS are vital for planning, monitoring and evaluation of health care delivery. The absence of formal OPD morbidity data flow further diminishes the key factor to estimate cost of OPD services in Sri Lanka (7). Need of a routine OPD morbidity data was repeatedly emphasized by researchers (8) and international organizations (9). Health system researchers investigate how health care is financed, organized, delivered and used in the process of achieving wider health and social goals. In this arena of research, this study explores the perception and feasibility of new out patients morbidity recording system introduced to OPD of public hospitals Sri Lanka as a systematic intervention.
Methodologies used for data generation depend on the organization’s needs. Morbidity data is often recorded as standard codes. Classification of diseases is a standard diagnostic tool, used to monitor the incidence and prevalence of diseases and other health problems or populations. ICPC (International Classification of Primary Care), which is an adaptation of International Classification of Diseases (ICD) (2) has achieved recognition as suitable for a General Practice (GP) (10). ICPC-2 is the most commonly used system in GP software (11) and useful in monitoring OPD functions (12). ICPC is recommended as a new analysis tool and is validated as a useful tool in a number of research projects (13). ICPC had been incorporated for morbidity surveys in many countries and had shown very effective (14-16). All studies given above were operated in electronic version of ICPC-2 software systems, but OPD in Sri Lankan hospitals depends mainly on paper-based manual systems. Since manual records carry many inherent limitations, developing a user friendly manual OPD morbidity recording system was a challenge.
Methods
We formulated an intervention study with three stages incorporated with mix method research design.
- Pre-intervention: development of new paper based OPD morbidity recording system;
- Intervention: implementation of new paper based OPD morbidity recording system in sample of hospitals;
- Post-intervention: feasibility assessment of the new paper based OPD morbidity recording system.
Pre-intervention
Development and designing of the new manual OPD morbidity recording system was done in this phase. A convenient sample representing all relevant stakeholders from policy level administrators, middle managers to operational level were included. OPD medical officers (MO/OPD), medical record officers (MRO), officers in registration table, officers in Medical Statistics Unit (MSU) were invited for discussions. Series of iterative open Delphi interviews, in-depth-interviews and focus group discussions were conducted as consultative discussions. A new ‘OPD form’, ‘OPD return’ and ‘Tally sheet’ with a documented training plan for orientation were formulated as part of a new morbidity recording system. The new recording system with its format designs were finalized with everybody’s consensus at the final workshop. New system was pretested in a peripheral hospital and altered for improvements.
Intervention
Three hospitals were selected randomly from all hospitals under the preview of Regional Director of Health Services Colombo representing each level; Primary Health Care Unit (PMCU), Divisional Hospitals (DH) and Base Hospitals (BH). All permanent staff working in OPD of selected hospitals were recruited for the study. Orientation to new process was done to all staff with a classroom training followed with one-week on-the-job training. Identification data and demographic information of the OPD form was filled by nurses and health assistants in registration table. Morbidity related information; patient’s history & examination and provisional/definitive diagnosis with ICPC-2 coding and treatments were recorded by MO/OPD in the same OPD form at consultation tables. All OPD forms were daily collected from the pharmacy counter and sent to medical record office in hospital as a monthly bundle. Hands-on-training for transferring data from OPD forms to tally sheets and completing the monthly OPD return was practiced for MRO. After adequate familiarization, the new OPD morbidity recording system was implemented for one-month duration in all 3 hospital OPD.
Post-intervention
Feasibility assessment was conducted at this phase and following quantitative and qualitative evaluations were carried out.
- Statistical analysis of the satisfaction of MO/OPD towards new OPD form using self-administered questionnaire;
- Quantitative analysis of accuracy & completeness of the entered OPD forms using observation check list;
- Average time taken to fill the new OPD form by time measuring check list;
- Qualitative assessment of new OPD morbidity recording system with staff involved to the process by focus group discussions.
Results
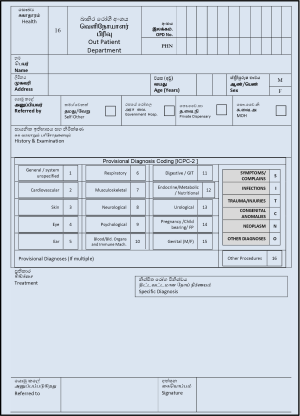
Qualitative discussions conducted at pre-intervention stage concluded with formulating a standard paper based OPD morbidity recording system. It consisted with ‘OPD form’ (Figure 1) which is to be completed at the registration table and consultation table. An ‘OPD return’ (Figure S1), a consolidated data entry form which is to be completed by MRO using the ‘Tally sheet’ (Figure S2) at record room. Induction training was designed to introduce the new recording system to all OPD and medical record office staff.
After the novel OPD morbidity recoding system was allowed to execute for one-month period, perception of MO/OPDs was assessed using a self-administered questionnaire. Basic demographic and work-related characteristics of the sample MO/OPDs working in hospitals were given Table 1. Eighty percent of MO/OPDs had 10 years or more experience as an MO. User satisfaction towards new OPD form was measured in five dimensions; user-friendly layout, perceived time to complete the form, technical competency to fill the form, adequacy of induction training and overall Satisfaction (Table 2). Overall satisfaction was very high (98%) and users were satisfied more than 95% with all the dimensions except for ‘Technical Competency’ (75%) (Table 2). Measurement of “Technical Competency” who are satisfied and not satisfied was statistically tested against work experience in Table 3 to figure out any association. There was no significant difference in satisfaction pertaining to “Technical Competency” of MO/OPD over work experience.
Table 1
| Character | Number (n=40) | Percentage |
|---|---|---|
| Age | ||
| 30 to <40 years | 11 | 27.5 |
| 40 to <50 years | 13 | 32.5 |
| 50 years or more | 16 | 40.0 |
| Sex | ||
| Male | 18 | 45.0 |
| Female | 22 | 55.0 |
| Work experience in public service | ||
| Up to 10 years | 08 | 20.0 |
| More than 10 years | 32 | 80.0 |
MO, medical officers; OPD, Out Patient Department.
Table 2
| Dimensions of satisfaction measured towards the use of OPD form | Number satisfied (n=40) | Percentage |
|---|---|---|
| User-friendly layout | 40 | 97.0 |
| Perceived time to complete | 39 | 97.5 |
| Technical competency to fill the form | 30 | 75.0 |
| Adequacy of induction training | 40 | 98.0 |
| Overall satisfaction | 40 | 98.0 |
MO, medical officers; OPD, Out Patient Department.
Table 3
| Level of satisfaction | Working experience | Significance | |
|---|---|---|---|
| ≤10 years | >10 years | ||
| Satisfied pertaining to technical competency | 5 (62.5%) | 25 (78.1%) | 0.387* |
| Not satisfied pertaining to technical competency | 3 (37.5%) | 7 (21.9%) | |
| Total | 8 (100%) | 32 (100%) | Not significant |
*, Fisher’s exact. OPD, Out Patient Department.
Entries made in all filled OPD forms were statistically analyzed for completeness. All hospitals showed more than 90% of overall completeness at registration table (Table 4). The overall completeness of the entries made in OPD form at the consultation table showed in PMCU: 95.1%, DH: 86.2% and BH: 68.3% for each hospital and overall completeness is declining when hospital becomes larger with the number of OPD patients (Table 5). Accuracy of entered ICPC-2 codes by MO/OPDs along with the patient disease presentation showed correct in almost all the cases (Table 6). Average time taken to fill the OPD form was less than 7 minutes (Table 7).
Table 4
| Type of hospital | Overall completeness* (%) | 95% confidant interval (CI) |
|---|---|---|
| PMCU (n=806) | 98.8 | 98.05–99.55 |
| DH (n=6,512) | 96.2 | 95.74–96.66 |
| BH (n=33,982) | 91.2 | 90.90–91.50 |
*, entries: date, OPD number, name, sex and address of OPD patients. OPD, Out Patient Department; PMCU, Primary Health Care Unit; DH, Divisional Hospitals; BH, Base Hospitals.
Table 5
| Type of hospital | Percentage completeness* (%) | 95% CI |
|---|---|---|
| PMCU (n=806) | 95.1 | 93.61–96.59 |
| DH (n=6512) | 86.2 | 85.36–87.04 |
| BH (n=33,982) | 68.3 | 67.80–68.80 |
*, history & examination, diagnosis code (ICPC-2) and treatment. OPD, Out Patient Department; PMCU, Primary Health Care Unit; DH, Divisional Hospitals; BH, Base Hospitals.
Table 6
| Aspect of accuracy | Number of patients (n=80) |
|---|---|
| Accurately entered | 79 (98.8%) |
| Not accurate | 1 (1.3%) |
| Total | 80 (100%) |
MO, medical officers; OPD, Out Patient Department.
Table 7
| Activity | Average time in minutes (n=80) (95% CI) |
|---|---|
| At the registration table | 2.2 (1.9–2.5) |
| At the consultation table | 4.0 (3.6–4.3) |
OPD, Out Patient Department.
Qualitative assessment revealed fact that new morbidity recording system is user friendly and MO/OPD could easily adapt with ICPC-2 coding for diagnosis. MRO informed that absence of converting diagnoses to codes during preparation of OPD return is well acceptable and convenient comparing to the problems experienced in Indoor Morbidity & Mortality Return (IMMR) recording. Apart from that, new OPD morbidity recording system has made MO/OPDs more conscious and accountable during consultation leading to rational prescribing.
Discussion
OPD is a vibrant place in a hospital. This project involved various stakeholders from all levels during the pre-intervention. Qualitative research methods allowed building consensus through communicating, sharing and problem-solving dialogues during the design stage of the project. Facilitating stakeholders to contribute during implementing novel systems minimize the resistance or unpredictable failure in future (17). Personnel Health Number (PHN) which is to be introduced to the hospital system in near future was also incorporated to OPD form in order to ease the data tracking (18).
Feasibility assessment which was carried out in the post-intervention, consisted with quantitative analysis and qualitative discussions to made rigor for evidence (19). Assessment of Perception of MO/OPD towards new OPD morbidity recoding system showed high overall satisfaction (98%). “Technical competency” which showed lower satisfaction can be attributed to MO/OPD unfamiliarity to a new coding system. This has been identified as an expected behavior in innovative approaches of work settings which needs to be managed carefully (20,21).
Completeness of filled new OPD form entries made at the registration table was high (>90%) in all three types of hospitals. ‘History & Examination’, ‘Treatment’ and ‘Diagnosis’ related entries were well recorded at the consultation table, but high variability (71–95%) in completeness of “diagnosis” was shown in the entries made at consultation table. A systematic review also has reported 67–99% variation in morbidity recording while carrying high overall completeness (22). Complement with above result, two Sri Lankan studies also have demonstrated 88.3% OPD morbidity records in hospitals at Polonnaruwa region and 50–70% in OPD of General Hospital Trincomalee (23) which were investigated in computerized OPDs. MO/OPD showed very high accuracy (99%) in direct manual entering of ICPC-2 codes (Table 6). ICPC-2 had been tested and found to be practical and reliable in general practice with less than 3% recoding errors (24). Some authors argue that accuracy may depend on the level of coding, whereas chapter heading for ICPC diagnoses carries high acccuracy (22,25). This intervention had only been used to record chapter headings due to the limitation of paper based entering forms.
‘Physician time’ had been considered as a demanding resource which can make major bad effects on the patient-doctor relationship (26). Timeliness for completion of OPD form was a major concern in this study due to the high work load and long queues in OPDs. Time spent at registration table with new recording system was not different from previous practice time. There was no perceived difference for average time spent at consultation table within two systems (Table 2). Adequate training is recommended before practice for successful results (27) before introducing novel systems. MROs were positive towards the new OPD return and tally sheet due to absence of code conversion, because the reliability of the data extraction for coding from medical records has reported as questionable (28). Tally sheet had made them easy to consolidate data, where there are no computer facilities. The goal of recording and adapting OPD morbidity data to the HMIS is to use them for decision making (29). Framework for conceptualizing and measuring implementation outcomes based on variables such as ‘acceptability’, ‘appropriateness’ and ‘feasibility’ (30), which were achieved in this study are the recommendations by WHO as the base for a successful implementation.
Conclusions
Results of the qualitative and quantitative assessments demonstrated that new paper based OPD morbidity recording system was well acceptable and feasible to implement in OPD settings and able to adapt with the HMIS. All staff working in OPD and record rooms were satisfied with the orientation training provided in introducing new recording system.
Recommendations
This research covered three levels of hospitals: PMCU, DH, BH with successful results, it is recommended to implement the new paper based OPD morbidity recording system to all hospital network step-wise along with orientation training. The readiness of the HMIS in MSU to respond to a large volume of data load from OPDs should be improved before implementation of the novel system. Include ICPC classifications for undergraduate curriculum is recommended to assure the technical quality in morbidity coding in future and it enables gradual omission of the orientation training for Medical Officers in future. Possibility of incorporating IT solutions with electronic version of ICPC to OPD units should be explored and researched in future.
Post-project sustainability measurements
Details of new paper based OPD morbidity recording system was forwarded to the National Drugs & Therapeutic Committee (NDTC) and recommended up in the Technical Advisory Committee (TAC) through Director Health Information with the concurrence of the Director General of Health Services in Ministry of Health Sri Lanka. Principal investigator presented the results to the executive committee and obtained approval for new recording system to be implemented in all hospitals in Sri Lanka. The responsibility of launching the new system was delegated to Health Information Unit at Ministry of Health. The up lifting the capacity of the MSU is being discussed and the procurements are to be commenced with the Second Health Sector Development Project (SHSDP) project allocations.


Acknowledgments
I would like to thank Dr. PG Maheepala, Former Director General Health Services, Ministry of Health Sri Lanka and the team of Medical officer Bio-informatics attached to Medical Statistics Unit (MSU), Ministry of Health for the guidance & constructive criticism made to this project a success.
Funding: The total budget for the research project was supported by the government of Sri Lanka (GOSL funds) as a research grant through Medical Research Institute (MRI), Sri Lanka (No. 09/2015).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jhmhp.2019.09.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethical clearance was obtained from Ethical Research Committee, Medical Research Institute, Sri Lanka (No. 09/2015). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Formal approval was granted by Director General Health Services in Ministry of Health followed with relevant institutional heads for the pilot study. Since intervention was only a process improvement tool, there was no anticipated risk to patients. Participants were well informed, trained and written consent was obtained for participation & publication. The permission for copy righting of ICPC was freely granted for research use by World Organization of Family Doctors (WONCA) Classification Committee.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kansal S, Kumara A, Singh I, et al. A study on morbidity pattern in rural community of eastern Uttar pradesh. Indian J Prev Soc Med 2008;39:184-8.
- PH3C Primary Health Care Classification Consortium. An introduction to ICPC-2 (2004). Available online: http://www.ph3c.org/4daction/w3_CatVisu/en/-an-introduction-to-icpc-2--2004.html?wDocID=98 (Accessed: 20th May 2015).
- Ministry of Health. Annual Health Bulletin, 1 ed. Medical Statistics Unit, Ministry of Health, Nutrition and Indigenous Medicine: Ministry of Health; 2015.
- Ministry of Health. Annual Health Bulletin, 1 ed. Medical Statistics Unit, Ministry of Health, Nutrition and Indigenous Medicine: Ministry of Health; 2012.
- Department of Health Services. Annual Health Bulletin, 1 ed. Colombo: Department of Health; 2003.
- Wijewardene K, Mohideem MR, Mendis S, et al. Prevalence of hypertension, diabetes and obesity: baseline findings of a population based survey in four provinces in Sri Lanka. Ceylon Med J 2005;50:62-70. [Crossref] [PubMed]
- Dharmarathne S, Agampodi S, Dasanayake S, et al. Disease burden assessment beyond in-patient data: A morbidity profile assessment of out patients. Intern J Prev Med 2005;3:730-2.
- Farnando G, A survey on morbidity patterns and drug requirements at the primary health care level, Sri Lanka. Essential Drug Monitor. Available online: http://apps.who.int/medicinedocs/en/m/abstract/Js21190en/ (Accessed: 12th February 2015).
- WHO/SEARO. Medicine in Health Care Delivery Sri Lanka: Situational Analysis: WHO/SEARO; 2016. Available online: http://www.searo.who.int/entity/medicines/sri_lanka_mar_2016.pdf?ua=1 (Accessed: 10th February 2016).
- Lamberts H, Okkes I. International Classification of Primary Care. [Published 2003]. Available online: http://www.kith.no/upload/1785/ICPC%20tutorial.ppt#374,15 (Accessed: 11th March 2015).
- The WONCA International Classification Committee. International Classification of Primary Care, Revised 2nd ed. New York: Oxford University Press; 2005.
- Wun Y, Lu X, Liang W, et al. The work by the developing primary care team in China: a survey in two cities. Fam Pract 2000;17:10-5. [Crossref] [PubMed]
- Family Medicine Research Centre; University of Sydney. ICPC-2 - International Classification for Primary Care. Available online: https://sydney.edu.au/medicine/fmrc/icpc-2/index.php (Accessed: 20th March 2016).
- Sinnadurai JT, Sivasampu S, Pin GP. 2016. National Medical Care Statistics 2014, 1st edn., Kuala Lumpur: The National Healthcare Statistics Initiative (NHSI). Available online: http://www.crc.gov.my/nhsi/wp-content/uploads/publications/nmcs2014/NMCS_2014_fullreport.pdf (Accessed: 2nd April 2016).
- Teng CL, Aljunid SM, Cheah M, et al. Morbidity and process of care in urban Malaysian general practice. Med J Malaysia 2003;58:365-74. [PubMed]
- Mash B, Fairall L, Adejayan OI, et al. A morbidity survey of South African primary care. PLoS One 2012;7:e32358 [Crossref] [PubMed]
- Brugha R, Varvasovsky Z. Stakeholder analysis: A review. Health Policy Plan 2000;15:239-46. [Crossref] [PubMed]
- Weerabaddana C, Wikramasinghe S, Rathnayake D, et al. Unique Health Identifier for all: Sri Lanka. Sri Lanka Journal of Medical Administration 2015;17:11-3.
- Curry LA, Nembhard IM, Bradley EH. Qualitative and Mixed Methods Provide Unique Contributions to Outcomes Research. Circulation 2009;119:1442-52. [Crossref] [PubMed]
- Herzberg F. One more time: How do you motivate employees. Haword Business Review 1968;01:46-57.
- Ramsay H, Scholarios D, Harley B. Employees and High-Performance Work Systems: Testing inside the black box. Br J Indust Relat 2000;38:501-31. [Crossref]
- Jordan K, Porcheret M, Croft P. Quality of morbidity coding in general practice computerized medical records: a systematic review. Fam Pract 2004;21:396-412. [Crossref] [PubMed]
- Jayawardena AS. The Electronic Hospital Information System Implemented at the District General Hospital Trincomalee-An Experience of Business Process Reengineering. J Community Med Health Educ 2014; [Crossref]
- Dungen C. Explaining variations in morbidity estimates: Data from general practice registration networks. Enschede: Ipskamp Drukkers; 2015. Available online: https://research.tilburguniversity.edu/en/publications/explaining-variations-in-morbidity-estimates-data-from-general-pr (Accessed: 15th February 2015).
- Britt H, Angelis M, Harris E. The reliability and validity of doctor-recorded morbidity data in active data collection systems. Scand J Prim Health Care 1998;16:50-5. [Crossref] [PubMed]
- Dugdale DC, Epstein R, Pantilat SZ. Time and the Patient–Physician Relationship. J Gen Intern Med 1999;14:S34-40. [Crossref] [PubMed]
- Hassey A, Gerrett D, Wilson A. A survey of validity and utility ofelectronic patient generated recordsin a general practice. BMJ 2001;322:1401-5. [Crossref] [PubMed]
- Britt H, Meza R, DelMar C. Methodology of morbidity and treatment data collection in general practice in Australia: a comparison of two methods. Fam Pract 1996;13:462-7. [Crossref] [PubMed]
- de Lusignan S, Weel C. The use of routinely collected computer data for research in primary care: opportunities and challenges. Fam Pract 2006;23:253-63. [Crossref] [PubMed]
- Peters DH, Adam T, Alonge O, et al. Implementation research: what it is and how to do it. BMJ 2013;347:f6753. [PubMed]
Cite this article as: Rathnayake D, Wikramasinghe C, Weerabaddana C. Introduce new paper-based outpatient morbidity recording system to outpatient departments of public hospitals in Sri Lanka: feasibility study. J Hosp Manag Health Policy 2019;3:27.

