
Combining standard psychiatric care with e-health follow up solutions—a viewpoint on making psychiatric care cost-effective for millions of patients and professionally satisfactory for providers
To illustrate the primary context of this article, let us discuss in detail a model of delivering e-health psychiatric intervention, outlined in Figure 1. In this model, our assumption is, as follows: patients cannot afford outpatient psychiatric care, so they search for health information online. To help these individuals, we can equip them with online resources to perform initial self-diagnosis, based on self-reported symptoms. Subsequently, the system could make automatic recommendations about the specific specialist who can treat their symptoms; this pre-selected provider can offer long-term follow up care, using e-health solutions that allow the patient to feel incentivized to remain under the supervision of a dedicated provider, without being discouraged by the financial burden of regular, outpatient office visits.
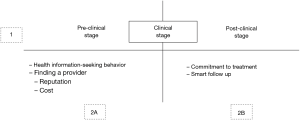
Point 1 denotes an arbitrary division of delivery of care into three stages: pre-clinical, clinical, and post-clinical; pre-clinical phase means that the patient is exploring her or his options regarding e-health psychiatric solutions; clinical stage is when the patient meets with a physician to discuss mixed-approach psychiatric care (outpatient and e-health follow up); post-clinical phase is the care experienced after initial appointment with the physician, delivered entirely in the e-health mode.
Point 2A concerns the pre-clinical stage, characterized by having the patient explore e-health options available to them. At this point, most patients use the Internet to research what e-health is, and how it can help them ameliorate symptoms associated with having a mental condition. Most individuals are reluctant to seek help in an outpatient setting, so they decide to find more information about their symptoms online. To accomplish this goal, they access discussion forums, health sites, networking websites, and online chat rooms to explore their symptoms together with other people who think they have a mental disorder. In this exploratory phase, people learn about their symptomology and continue to re-evaluate possible coping strategies that do not involve seeing a physician in person just yet. However, given strong marketing for self-help websites and mobile apps, some of these patients will gravitate toward exploring e-health interventions; of those, most will attempt subscribing to at least one of these self-help products, hoping for improvement. If that fails, they are more likely to seek help from a psychiatrist but will realize two primary obstacles—the cost of treatment and stigmatization associated with receiving mental health treatment.
One of the reasons why people choose to search for health information online is that it’s free; they hope to find answers to questions that a doctor might address right away, but charges for that information significantly more than the cost of self-directed online research. That searching for health advice is, in itself, an e-health intervention, intended to mitigate the unexplainable symptomology of an undiagnosed mental condition. For some patients, this approach of self-healing will be sufficient; some will become addicted to using the internet to search for health information; others will get scared by some untruthful health advice, promoting them to seek clarification with a healthcare provider; yet others will purchase a self-help product, as it will generally cost much less than attending a consultation with a physician. Regardless of choices, technology creates an incentive for both searching health advice and using unverified health promotion products. This creates an opportunity for physicians to combine their expertise with these market needs to offer cost-effective solutions.
Point 2B, which denotes the post-clinical stage, offers physicians the opportunity to work with patients trapped in the pre-clinical, self-help stage of treatment. These patients are typically too fearful of facing the cost associated with traditional treatment model (that is: the patient experiences worrisome symptoms, goes to the physician, pays for services, receives treatments, follows up with the physician, and covers any extra cost associated with receiving treatment). The goal of the proposed model is to bridge this gap, by combining traditional outpatient treatment with expanded follow-up care, facilitated through e-health interventions. This allows patients to receive a consultation with the doctor, while continuing treatment through cost and time effective follow-ups, offered online through the doctor’s communication website, or third-party solutions.
The reason why this solution is ideal, yet rarely exercised, is two-fold. First, the patient gets to explore his or her symptoms online and, based on specific online tools, gets connected to a nearby psychiatric specialist who provides care in patient’s areas of health concern; at this point, the patient also considers what past patients have said about the physician (to determine whether the doctor is the right match for them, both expertise-wise and financially). Second, the patient connects with the doctor, attends a consultation in person, receives the diagnosis and treatment plan, and enters into long-term follow-up e-care (should she or he require long-term treatment).
Ordinarily, psychiatrists prefer to see their patients at regular intervals to revised treatment; this approach works well for patients that can afford it. In a proposed model, the patient gets to ask questions and raise concerns through an online follow-up system; the doctor responds to these concerns promptly by, for instance, sending brief voice memo responses or remotely adjusting medication list, based on self-reported symptoms. This way, the doctor can maximize his or her outpatient practice—continue to see full-time patients that can afford office visits, and provided responses and medication management to a large group of patients who are receiving treatment in the e-therapy mode.
At first sight, it might look like the doctor provides e-therapy as a sort of part-time duty; while this is, to some degree, correct—the patient benefits from knowing that they are assigned to a qualified clinician for long-term care and may, for a low maintenance fee, follow up with their provider at their convenience.
The proposed solution creates an incentive for patients who are perpetually engaging in online health information seeking behavior but are resistant to accessing care in the outpatient clinic. Therefore, to popularize these solutions, it is essential to accomplish three goals. First, we need to create online health resources that allow patients to explore psychiatric symptoms and, based on their self-reported concerns, get provider recommendations. Second, the provider must be willing to compromise on the standard of care to expand access to a more significant number of patients, who may not want to come into the office for regular follow-ups. Third, the provider and the patient should be able to form a trusting relationship that extends beyond the confines of the doctor’s office—and forage into the e-therapy mode. These solutions allow the physicians to maintain busy practice by providing care to long-term patients while acting remotely as information liaison and treatment provider to those patients who are unable to afford regular, in-person follow-ups.
The apparent obstacle of the proposed model is ethical standards. How are we going to make sure that providers provide compassionate and adequate care when caring for a patient in ad hoc, e-therapy mode? What is the fair pricing for such remote care? What about the side effects of treatment—it might be unsafe to rely on remote monitoring? These are some of the concerns that would require clarification. Nevertheless, currently, there are numerous efforts of implementing e-health solutions in various medical specialties. Psychiatry is the next natural group of healthcare providers that need to consider how using technology can connect mental health providers with patients while making services affordable. Lastly, the proliferation of mobile apps that offer psychological counseling might foreshadow the benefits of outpatient treatment; therefore, psychiatrists need to think about expanding their care outside of their comfort zone and into the digital space.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a unsolicited submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jhmhp.2018.07.07). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Cite this article as: Sendler DJ. Combining standard psychiatric care with e-health follow up solutions—a viewpoint on making psychiatric care cost-effective for millions of patients and professionally satisfactory for providers. J Hosp Manag Health Policy 2018;2:40.

